Inflammatory Responses Induced by Bacteria - CEMIR
Inflammatory Responses Induced by Bacteria
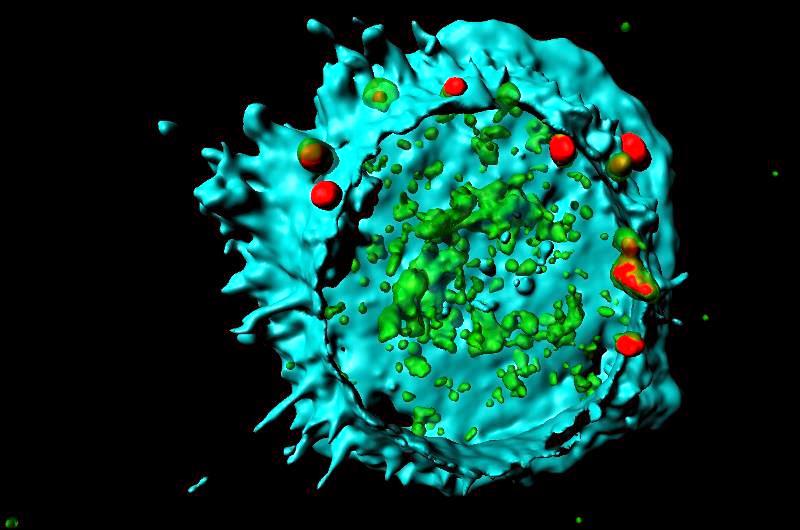
Identification of Vesicle Transport Components and Signalling Pathways that regulate Interferon Responses from Endosomes.
In the presence of systemic infection, microbial pathogens induce strong inflammatory- and coagulation activation, leading to sepsis and septic shock.
Also, an anti-inflammatory response is induced during sepsis that can contribute to secondary infections. Severe bacterial infections may lead to high amounts of type I IFNs that can result in production of immunosuppressive molecules increasing the risk for secondary infections.
26 Feb 2018
The main aim of this theme is to find new principles of Toll-like receptor (TLR) signalling resulting in type I interferons from endosomes and phagosomes. A second aim is to find ways to inhibit inflammatory responses by targeting TLRs and the complement system.
Major achievements
- Generated recombinant anti-porcine and anti-human CD14 Abs endowed with the IgG2/IgG4 hybrid Fc region. These Abs are unique tools for future studies of CD14 inhibition using porcine in vivo models, and pave the way for human therapy with CD14 inhibition, preferentially in combination with complement inhibition.
- Published data suggesting that specific blockade of CD14 and complement factor C5 represents a promising new therapeutic strategy for treatment of polymicrobial sepsis.
- Published data demonstrating that inhibiting complement and CD14 efficiently attenuated Staphylococcus aureus – induced inflammation.
- Published data showing that Rab11a regulates TLR4 mediated IFN-β production through its ability to transport TRAM form Golgi to ERC and further onto endosomes.
- Demonstrated a physiological role of TLR8 in the sensing of entire S. aureus in human primary phagocytes, including the induction of IFN-β and IL-12 production via a TAK1 -: IKKβ -: IRF5 pathway that can be inhibited by TLR2 signaling.
- Published data showing that combined inhibition of complement factor C5 and CD14 significantly improved survival, hemodynamic parameters and inflammation in a blinded, randomized trial of porcine polymicrobial sepsis.
- Published data demonstrating that human endothelial cell activation by E. coli and S. aureus is mediated by TNF and IL-1β secondarily to activation of C5 and CD14 in whole blood. Thus, both upstream combined targeting of C5 and CD14 and downstream combined targeting of TNF and IL-1β appear to be promising foci to modulate EC activation in inflammation.
- Published results showing a novel function of TRAM and TRIF in TLR2-mediated signal transduction.
- Demonstrated that whole bacteria-induced inflammation was inhibited more efficiently by anti-CD14 than by the TLR4 antagonist eritoran, particularly when combined with complement inhibition. The data suggest that combined CD14 and complement inhibition may prove a promising treatment strategy for bacterial sepsis.
- Established that TLR8 is a major sensor for Group B Streptococci in human macrophages.
- Produced experimental data showing that CD150 plays an essential role in regulating TLR4-mediated TRIF-dependent signaling from gram-negative bacteria phagosomes in human macrophages. This makes CD150 a potential target for modulation of TLR4-dependent type I IFN expression.