Publications

Forskningsresultater fra Nor-COAST
Her presenterer vi resultater fra studiene våre i et lettlest format.
Articles published in 2021
Neopterin and kynurenic acid as predictors of stroke recurrence and mortality: a multicentre prospective cohort study on biomarkers of inflammation measured three months after ischemic stroke.
Neopterin and kynurenic acid as predictors of stroke recurrence and mortality: a multicentre prospective cohort study on biomarkers of inflammation measured three months after ischemic stroke.
Background: Chronic low-grade inflammation is associated with both ischemic stroke and sedentary behaviour. The aim of this study was to investigate the predictive abilities of biomarkers of inflammation and immune modulation associated with sedentary behaviour for ischemic stroke recurrence and mortality in a stroke population.
Methods: Patients admitted to hospital for acute stroke were recruited to the prospective multicentre cohort study, the Norwegian Cognitive Impairment After Stroke (Nor-COAST) study, from May 2015 until March 2017. Patients with ischemic stroke, blood samples available from the three-month follow-up, and no stroke recurrence before the three-month follow-up were included. Serum was analysed for C-reactive protein (CRP) with high-sensitive technique, and plasma for interleukin-6 (IL-6), neopterin, pyridoxic acid ratio index (PAr-index: 4-pyridoxic acid: [pyrioxal+pyridoxal-5′-phosphate]) and kynurenic acid (KA). Ischemic stroke recurrence and death were identified by the Norwegian Stroke Registry and the Cause of Death Registry until 31 December 2018.
Results: The study included 354 patients, 57% male, mean age 73 (SD 11) years, mean observation time 2.5 (SD 0.6) years, and median National Institute of Health Stroke Scale of 0 (IQR 1) at three months. CRP was associated with mortality (HR 1.40, CI 1.01, 1.96, p = 0.046), and neopterin was associated with the combined endpoint (recurrent ischemic stroke or death) (HR 1.52, CI 1.06, 2.20, p = 0.023), adjusted for age, sex, prior cerebrovascular disease, modified Rankin Scale, and creatinine. When adding neopterin and KA to the same model, KA was negatively associated (HR 0.57, CI 0.33, 0.97, p = 0.038), and neopterin was positively associated (HR 1.61, CI 1.02, 2.54, p = 0.040) with mortality. Patients with cardioembolic stroke at baseline had higher levels of inflammation at three months.
Conclusion: Neopterin might be a valuable prognostic biomarker in stroke patients. The use of KA as a measure of anti-inflammatory capacity should be investigated further.
Journal: BMC Neurology
Published 8 December 2021
Risk stratification in patients with ischemic stroke and residual cardiovascular risk with current secondary prevention.
Risk stratification in patients with ischemic stroke and residual cardiovascular risk with current secondary prevention.
 Purpose: Suboptimal secondary prevention in patients with stroke causes a remaining cardiovascular risk desirable to reduce. We have validated a prognostic model for secondary preventive settings and estimated future cardiovascular risk and theoretical benefit of reaching guideline recommended risk factor targets.
Purpose: Suboptimal secondary prevention in patients with stroke causes a remaining cardiovascular risk desirable to reduce. We have validated a prognostic model for secondary preventive settings and estimated future cardiovascular risk and theoretical benefit of reaching guideline recommended risk factor targets.
Patients and Methods: The SMART-REACH (Secondary Manifestations of Arterial Disease-Reduction of Atherothrombosis for Continued Health) model for 10-year and lifetime risk of cardiovascular events was applied to 465 patients in the Norwegian Cognitive Impairment After Stroke (Nor-COAST) study, a multicenter observational study with two-year follow-up by linkage to national registries for cardiovascular disease and mortality. The residual risk when reaching recommended targets for blood pressure, low-density lipoprotein cholesterol, smoking cessation and antithrombotics was estimated.
Results: In total, 11.2% had a new event. Calibration plots showed adequate agreement between estimated and observed 2-year prognosis (C-statistics 0.63, 95% confidence interval 0.55– 0.71). Median estimated 10-year risk of recurrent cardiovascular events was 42% (Interquartile range (IQR) 32– 54%) and could be reduced to 32% by optimal guideline-based therapy. The corresponding numbers for lifetime risk were 70% (IQR 63– 76%) and 61%. We estimated an overall median gain of 1.4 (IQR 0.2– 3.4) event-free life years if guideline targets were met.
Conclusion: Secondary prevention was suboptimal and residual risk remains elevated even after optimization according to current guidelines. Considerable interindividual variation in risk exists, with a corresponding variation in benefit from intensification of treatment. The SMART-REACH model can be used to identify patients with the largest benefit from more intensive treatment and follow-up.
Journal: Clinical Epidemiology
Published 20th of August 2021
Predicting the Emergence of Major Neurocognitive Disorder Within Three Months After a Stroke.
Predicting the Emergence of Major Neurocognitive Disorder Within Three Months After a Stroke.
 Background: Neurocognitive disorder (NCD) is common after stroke, with major NCD appearing in about 10% of survivors of a first-ever stroke. We aimed to classify clinical- and imaging factors related to rapid development of major NCD 3 months after a stroke, so as to examine the optimal composition of factors for predicting rapid development of the disorder. We hypothesized that the prediction would mainly be driven by neurodegenerative as opposed to vascular brain changes.
Background: Neurocognitive disorder (NCD) is common after stroke, with major NCD appearing in about 10% of survivors of a first-ever stroke. We aimed to classify clinical- and imaging factors related to rapid development of major NCD 3 months after a stroke, so as to examine the optimal composition of factors for predicting rapid development of the disorder. We hypothesized that the prediction would mainly be driven by neurodegenerative as opposed to vascular brain changes.
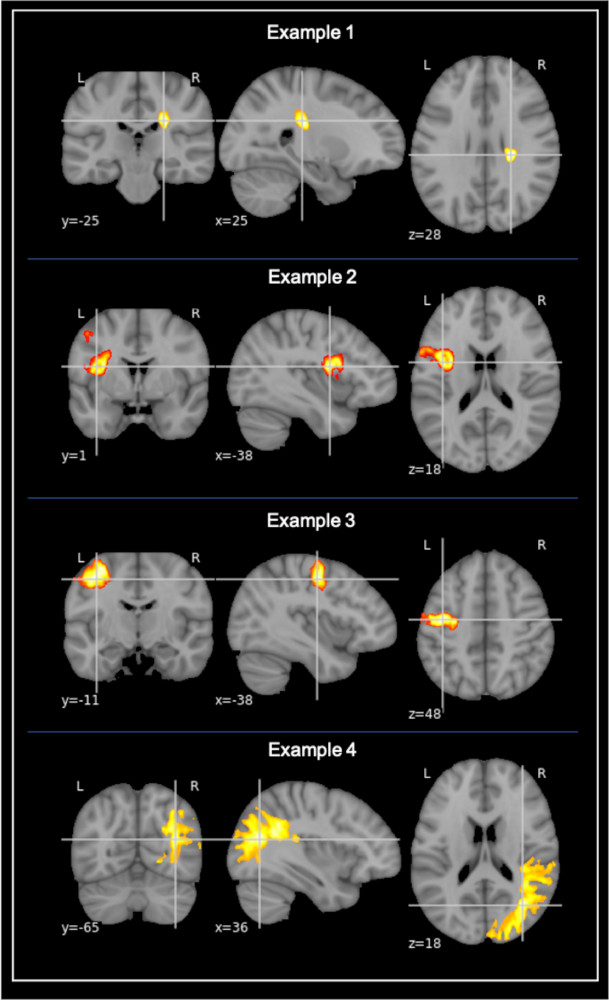
Methods: Stroke survivors from five Norwegian hospitals were included from the “Norwegian COgnitive Impairment After STroke” (Nor-COAST) study. A support vector machine (SVM) classifier was trained to distinguish between patients who developed major NCD 3 months after the stroke and those who did not. Potential predictor factors were based on previous literature and included both vascular and neurodegenerative factors from clinical and structural magnetic resonance imaging findings. Cortical thickness was obtained via FreeSurfer segmentations, and volumes of white matter hyperintensities (WMH) and stroke lesions were semi-automatically gathered using FSL BIANCA and ITK-SNAP, respectively. The predictive value of the classifier was measured, compared between classifier models and cross-validated.
Results: Findings from 227 stroke survivors [age = 71.7 (11.3), males = (56.4%), stroke severity NIHSS = 3.8 (4.8)] were included. The best predictive accuracy (AUC = 0.876) was achieved by an SVM classifier with 19 features. The model with the fewest number of features that achieved statistically comparable accuracy (AUC = 0.850) was the 8-feature model. These features ranked by their weighting were; stroke lesion volume, WMH volume, left occipital and temporal cortical thickness, right cingulate cortical thickness, stroke severity (NIHSS), antiplatelet medication intake, and education.
Conclusion: The rapid (<3 months) development of major NCD after stroke is possible to predict with an 87.6% accuracy and seems dependent on both neurodegenerative and vascular factors, as well as aspects of the stroke itself. In contrast to previous literature, we also found that vascular changes are more important than neurodegenerative ones. Although possible to predict with relatively high accuracy, our findings indicate that the development of rapid onset post-stroke NCD may be more complex than earlier suggested.
Predicting the Emergence of Major Neurocognitive Disorder Within Three Months After a Stroke.
Journal: Frontiers in Aging Neuroscience
Published 16th of August 2021
Pre-stroke cognitive impairment is associated with vascular imaging pathology.
Pre-stroke cognitive impairment is associated with vascular imaging pathology.
Background: Chronic brain pathology and pre-stroke cognitive impairment (PCI) is predictive of post-stroke dementia. The aim of the current study was to measure pre-stroke neurodegenerative and vascular disease burden found on brain MRI and to assess the association between pre-stroke imaging pathology and PCI, whilst also looking for potential sex differences.
Methods: This prospective brain MRI cohort is part of the multicentre Norwegian cognitive impairment after stroke (Nor-COAST) study. Patients hospitalized with acute ischemic or hemorrhagic stroke were included from five participating stroke units. Visual rating scales were used to categorize baseline MRIs (N = 410) as vascular, neurodegenerative, mixed, or normal, based on the presence of pathological imaging findings. Pre-stroke cognition was assessed by interviews of patients or caregivers using the Global Deterioration Scale (GDS). Stroke severity was assessed with the National Institute of Health Stroke Scale (NIHSS). Univariate and multiple logistic regression analyses were performed to investigate the association between imaging markers, PCI, and sex.
Results: Patients' (N = 410) mean (SD) age was 73.6 (±11) years; 182 (44%) participants were female, the mean (SD) NIHSS at admittance was 4.1 (±5). In 68% of the participants, at least one pathological imaging marker was found. Medial temporal lobe atrophy (MTA) was present in 30% of patients, white matter hyperintensities (WMH) in 38% of patients and lacunes in 35% of patients. PCI was found in 30% of the patients. PCI was associated with cerebrovascular pathology (OR 2.5; CI = 1.4 to 4.5, p = 0.001) and mixed pathology (OR 3.4; CI = 1.9 to 6.1, p = 0.001) but was not associated with neurodegeneration (OR 1.0; CI = 0.5 to 2.2; p = 0.973). Pathological MRI markers, including MTA and lacunes, were more prevalent among men, as was a history of clinical stroke prior to the index stroke. The OR of PCI for women was not significantly increased (OR 1.2; CI = 0.8 to 1.9; p = 0.3).
Conclusions: Pre-stroke chronic brain pathology is common in stroke patients, with a higher prevalence in men. Vascular pathology and mixed pathology are associated with PCI. There were no significant sex differences for the risk of PCI.
Journal: BMC Geriatrics
Published 14th of June 2021
Impact of Vascular Risc Factors on Post-stroke Cognitive Impairments.
Impact of Vascular Risc Factors on Post-stroke Cognitive Impairments.
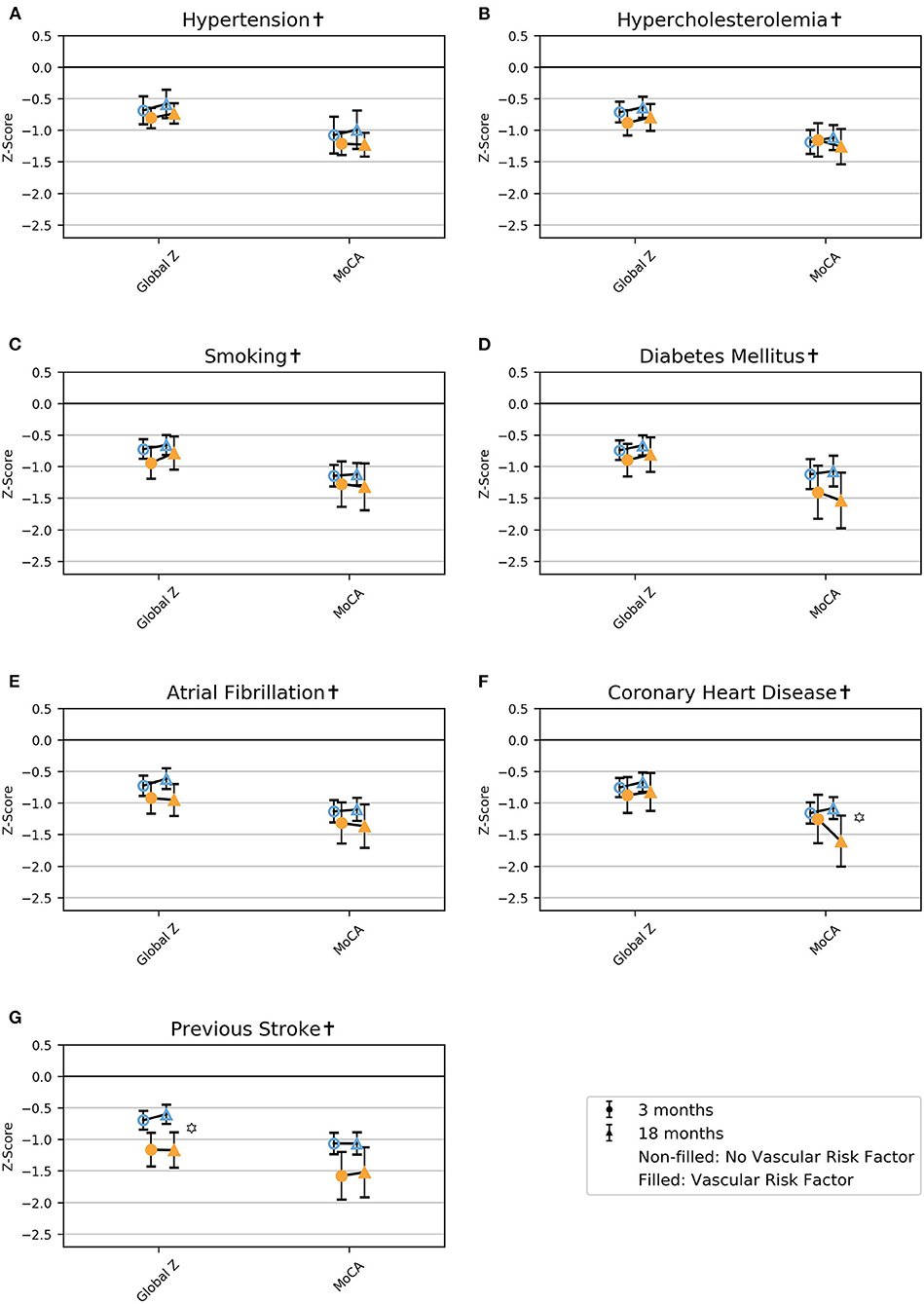 Introduction: Post-stroke cognitive impairment (PSCI) is common, but evidence on the impact of vascular risk factors is lacking. We explored the association between pre-stroke vascular risk factors and PSCI and studied the course of PSCI.
Introduction: Post-stroke cognitive impairment (PSCI) is common, but evidence on the impact of vascular risk factors is lacking. We explored the association between pre-stroke vascular risk factors and PSCI and studied the course of PSCI.
Materials and Methods: Vascular risk factors were collected at baseline in stroke survivors (n = 635). Cognitive assessments of attention, executive function, memory, language, and the Montreal Cognitive Assessment (MoCA) were performed at 3 and/or 18 months post-stroke. Stroke severity was assessed with the National Institutes of Health Stroke Scale (NIHSS). PSCI was measured with global z; MoCA z-score; and z-score of the four assessed cognitive domains. Mixed-effect linear regression was applied with global z, MoCA z-score, and z-scores of the cognitive domains as dependent variables. Independent variables were the vascular risk factors (hypertension, hypercholesterolemia, smoking, diabetes mellitus, atrial fibrillation, coronary heart disease, previous stroke), time, and the interaction between these. The analyses were adjusted for age, education, and sex. There were between 5 and 25% missing data for the variables for PSCI.
Results: Mean age was 71.6 years (SD 11.7); 42% were females; and the mean NIHSS score at admittance was 3.8 (SD 4.8). Regardless of vascular risk factors, global z, MoCA, and all the assessed cognitive domains were impaired at 3 and 18 months, with MoCA being the most severely impaired. Atrial fibrillation (AF) was associated with poorer language at 18 months and coronary heart disease (CHD) with poorer MoCA at 18 months (LR = 12.80, p = 0.002, and LR = 8.32, p = 0.004, respectively). Previous stroke was associated with poorer global z and attention at 3 and 18 months (LR = 15.46, p < 0.001, and LR = 16.20, p < 0.001). In patients without AF, attention improved from 3 to 18 months, and in patients without CHD, executive function improved from 3 to 18 months (LR = 10.42, p < 0.001, and LR = 9.33, p = 0.009, respectively).
Discussion: Our findings indicate that a focal stroke lesion might be related to pathophysiological processes leading to global cognitive impairment. The poorer prognosis of PSCI in patients with vascular risk factors emphasizes the need for further research on complex vascular risk factor interventions to prevent PSCI.
Impact of Vascular Risc Factors on Post-stroke Cognitive Impairments. The Nor-COAST study.
Journal: Frontiers in Neurology
Published 5th August 2021
Investigating novel biomarkers of immune activation and modulation in the context of sedentary behaviour.
Investigating novel biomarkers of immune activation and modulation in the context of sedentary behaviour.
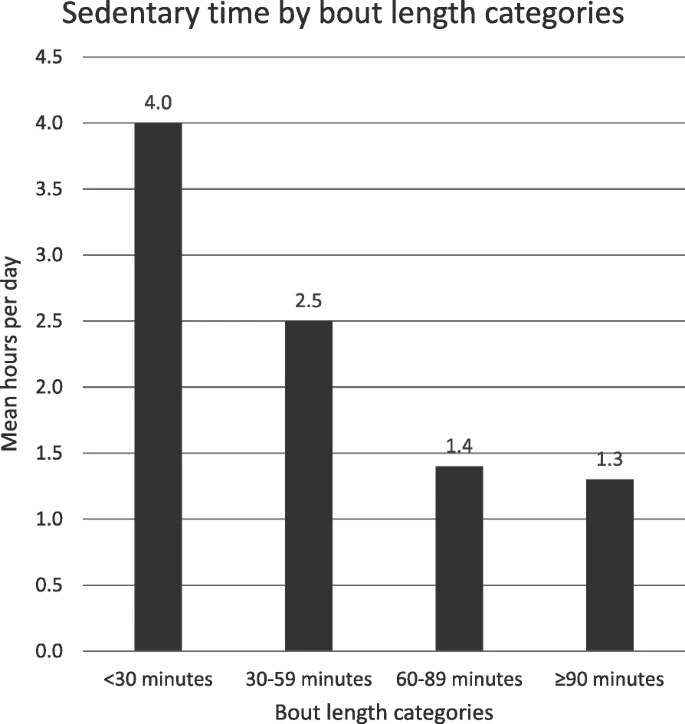 Background: Sedentary behaviour is associated with disease, but the molecular mechanisms are not understood. Valid biomarkers with predictive and explanatory properties are required. Therefore, we have investigated traditional and novel biomarkers of inflammation and immune modulation and their association to objectively measured sedentary behaviour in an ischemic stroke population.
Background: Sedentary behaviour is associated with disease, but the molecular mechanisms are not understood. Valid biomarkers with predictive and explanatory properties are required. Therefore, we have investigated traditional and novel biomarkers of inflammation and immune modulation and their association to objectively measured sedentary behaviour in an ischemic stroke population.
Methods: Patients admitted to hospital with acute ischemic stroke were included in the multicentre Norwegian Cognitive Impairment After Stroke (Nor-COAST) study (n = 815). For this sub-study (n = 257), sedentary behaviour was registered 3 months after stroke using position transition data from the body-worn sensor, ActivPal®. Blood samples were analysed for high sensitive C-reactive protein (hsCRP), the cytokines interleukin-6 (IL-6) and 10 (IL-10), neopterin, tryptophan (Trp), kynurenine (kyn), kynurenic acid (KA), and three B6 vitamers, pyridoxal 5′-phosphate (PLP), pyridoxal (PL), and pyridoxic acid (PA). The kynurenine/tryptophan ratio (KTR) and the pyridoxic acid ratio index (PAr = PA: PL + PLP) were calculated.
Results: Of the 815 patients included in the main study, 700 attended the three-month follow-up, and 257 fulfilled the inclusion criteria for this study. Sedentary time was significantly associated with levels of hsCRP, IL-6, neopterin, PAr-index, and KA adjusted for age, sex, waist circumference, and creatinine. In a fully adjusted model including all the significant biomarkers except hsCRP (because of missing values), sedentary time was independently positively associated with the PAr-index and negatively with KA. We did not find an association between sedentary behaviour, IL-10, and KTR.
Conclusions: The PAr-index is known to capture several modes of inflammation and has previously shown predictive abilities for future stroke. This novel result indicates that the PAr-index could be a useful biomarker in future studies on sedentary behaviour and disease progression. KA is an important modulator of inflammation, and this finding opens new and exciting pathways to understand the hazards of sedentary behaviour.
Journal: BMC Neurology
Published 16th of August 2021
Associaton between in-hospital frailty and health-related quality of life after stroke.
Associaton between in-hospital frailty and health-related quality of life after stroke.
Background: Stroke survivors are known to have poorer health-related quality of life (HRQoL) than the general population, but less is known about characteristics associated with HRQoL decreasing through time following a stroke. This study aims to examine how in-hospital frailty is related to HRQoL from 3 to 18 months post stroke.
Method: Six hundred twenty-five participants hospitalised with stroke were included and followed up at 3 and/or 18 months post stroke. Stroke severity was assessed the day after admission with the National Institutes of Health Stroke Scale (NIHSS). A modified Fried phenotype was used to assess in-hospital frailty; measures of exhaustion, physical activity, and weight loss were based on pre-stroke status, while gait speed and grip strength were measured during hospital stay. HRQoL at 3- and 18-months follow-up were assessed using the five-level version of the EuroQol five-dimensional descriptive system (EQ-5D-5L) and the EuroQol visual analogue scale (EQ-5D VAS). We conducted linear mixed effect regression analyses unadjusted and adjusted for sex, age, and stroke severity to investigate the association between in-hospital frailty and post-stroke HRQoL.
Results: Mean (SD) age was 71.7 years (11.6); mean NIHSS score was 2.8 (4.0), and 263 (42.1%) were female. Frailty prevalence was 10.4%, while 58.6% were pre-frail. The robust group had EQ-5D-5L index and EQ-5D VAS scores at 3 and 18 months comparable to the general population. Also at 3 and 18 months, the pre-frail and frail groups had significantly lower EQ-5D-5L indices than the robust group (p < 0.001), and the frail group showed a larger decrease from 3 to 18 months in the EQ-5D-5L index score compared to the robust group (− 0.056; 95% CI − 0.104 to − 0.009; p = 0.021). There were no significant differences in change in EQ-5D VAS scores between the groups.
Conclusion: This study on participants mainly diagnosed with mild strokes suggests that robust stroke patients have fairly good and stable post-stroke HRQoL, while post-stroke HRQoL is impaired and continues to deteriorate among patients with in-hospital frailty. This emphasises the importance of a greater focus on frailty in stroke units.
Journal: BMC Neurology
Published 4 of March 2021
Clinically accessible neuroimaging predictors of poststroke neurocognitive disorder.
Clinically accessible neuroimaging predictors of poststroke neurocognitive disorder.
Background: Neurocognitive disorder (NCD) is common in stroke survivors. We aimed to identify clinically accessible imaging markers of stroke and chronic pathology that are associated with early post-stroke NCD.
Methods: We included 231 stroke survivors from the “Norwegian Cognitive Impairment after Stroke (Nor-COAST)” study who underwent a standardized cognitive assessment 3 months after the stroke. Any NCD (mild cognitive impairment and dementia) and major NCD (dementia) were diagnosed according to “Diagnostic and Statistical Manual of Mental Disorders (DSM-5)” criteria. Clinically accessible imaging findings were analyzed on study-specific brain MRIs in the early phase after stroke. Stroke lesion volumes were semi automatically quantified and strategic stroke locations were determined by an atlas based coregistration. White matter hyperintensities (WMH) and medial temporal lobe atrophy (MTA) were visually scored. Logistic regression was used to identify neuroimaging findings associated with major NCD and any NCD.
Results: Mean age was 71.8 years (SD 11.1), 101 (43.7%) were females, mean time from stroke to imaging was 8 (SD 16) days. At 3 months 63 (27.3%) had mild NCD and 65 (28.1%) had major NCD. Any NCD was significantly associated with WMH pathology (odds ratio (OR) = 2.73 [1.56 to 4.77], p = 0.001), MTA pathology (OR = 1.95 [1.12 to 3.41], p = 0.019), and left hemispheric stroke (OR = 1.8 [1.05 to 3.09], p = 0.032). Major NCD was significantly associated with WMH pathology (OR = 2.54 [1.33 to 4.84], p = 0.005) and stroke lesion volume (OR (per ml) =1.04 [1.01 to 1.06], p = 0.001).
Conclusion: WMH pathology, MTA pathology and left hemispheric stroke were associated with the development of any NCD. Stroke lesion volume and WMH pathology were associated with the development of major NCD 3 months after stroke. These imaging findings may be used in the routine clinical setting to identify patients at risk for early post-stroke NCD.
Journal: BMC Neurology
Published 25th of February 2021
Associations between post-stroke motor and cognitive function.
Associations between post-stroke motor and cognitive function.
Background: Motor and cognitive impairments are frequently observed following stroke, but are often managed as distinct entities, and there is little evidence regarding how they are related. The aim of this study was to describe the prevalence of concurrent motor and cognitive impairments 3 months after stroke and to examine how motor performance was associated with memory, executive function and global cognition.
Methods: The Norwegian Cognitive Impairment After Stroke (Nor-COAST) study is a prospective multicentre cohort study including patients hospitalized with acute stroke between May 2015 and March 2017. The National Institutes of Health Stroke Scale (NIHSS) was used to measure stroke severity at admission. Level of disability was assessed by the Modified Rankin Scale (mRS). Motor and cognitive functions were assessed 3 months post-stroke using the Montreal Cognitive Assessment (MoCA), Trail Making Test Part B (TMT-B), 10-Word List Recall (10WLR), Short Physical Performance Battery (SPPB), dual-task cost (DTC) and grip strength (Jamar®). Cut-offs were set according to current recommendations. Associations were examined using linear regression with cognitive tests as dependent variables and motor domains as covariates, adjusted for age, sex, education and stroke severity.
Results: Of 567 participants included, 242 (43%) were women, mean (SD) age was 72.2 (11.7) years, 416 (75%) had an NIHSS score ≤ 4 and 475 (84%) had an mRS score of ≤2. Prevalence of concurrent motor and cognitive impairment ranged from 9.5% for DTC and 10WLR to 22.9% for grip strength and TMT-B. SPPB was associated with MoCA (regression coefficient B = 0.465, 95%CI [0.352, 0.578]), TMT-B (B = -9.494, 95%CI [− 11.726, − 7.925]) and 10WLR (B = 0.132, 95%CI [0.054, 0.211]). Grip strength was associated with MoCA (B = 0.075, 95%CI [0.039, 0.112]), TMT-B (B = -1.972, 95%CI [− 2.672, − 1.272]) and 10WLR (B = 0.041, 95%CI [0.016, 0.066]). Higher DTC was associated with more time needed to complete TMT-B (B = 0.475, 95%CI [0.075, 0.875]) but not with MoCA or 10WLR.
Conclusion: Three months after suffering mainly minor strokes, 30–40% of participants had motor or cognitive impairments, while 20% had concurrent impairments. Motor performance was associated with memory, executive function and global cognition. The identification of concurrent impairments could be relevant for preventing functional decline.
Associations between post-stroke motor and cognitive function: a cross-sectional study.
Journal: BMC Geriatrics
Published 5th February 2021
Test Accuracy of the Monteal Cognitive Assessment in Screening for Early Poststroke Neurocognitive Disorder.
Test Accuracy of the Monteal Cognitive Assessment in Screening for Early Poststroke Neurocognitive Disorder.
 Background and Purpose: We determined the diagnostic accuracy of the Montreal Cognitive Assessment (MoCA) for poststroke neurocognitive disorder defined according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria in a prospective observational study.
Background and Purpose: We determined the diagnostic accuracy of the Montreal Cognitive Assessment (MoCA) for poststroke neurocognitive disorder defined according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria in a prospective observational study.
Methods: Consecutive participants able to complete a cognitive test battery and MoCA 3 months poststroke were included. The reference standard of neurocognitive disorder was defined as a score of ≥1.5 SD below the normative mean in ≥1 cognitive domain on the cognitive test battery.
Results: Among 521 participants (43.6% women; mean age/SD, 71.5/12.0 years; mean education/SD, 12.4/3.8 years), the area under the receiver operating characteristic curve of MoCA for neurocognitive disorder was 0.80 (95% CI, 0.76–0.84). Using the standard MoCA cutoff <26, sensitivity was 0.71 (0.69–0.79) with specificity of 0.73 (0.66–0.76). MoCA cutoff of <27 gave higher sensitivity (0.82 [0.77–0.85]) at the expense of specificity (0.60 [0.53–0.66]).
Discussion: MoCA has reasonable accuracy for poststroke neurocognitive disorder diagnosed using the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, criteria.
Journal: Stroke
Published 30th of November 2020
Articles published in 2020
The Risk of Selection Bias in a Clinical Multi-Center Cohort Study.
The Risk of Selection Bias in a Clinical Multi-Center Cohort Study.
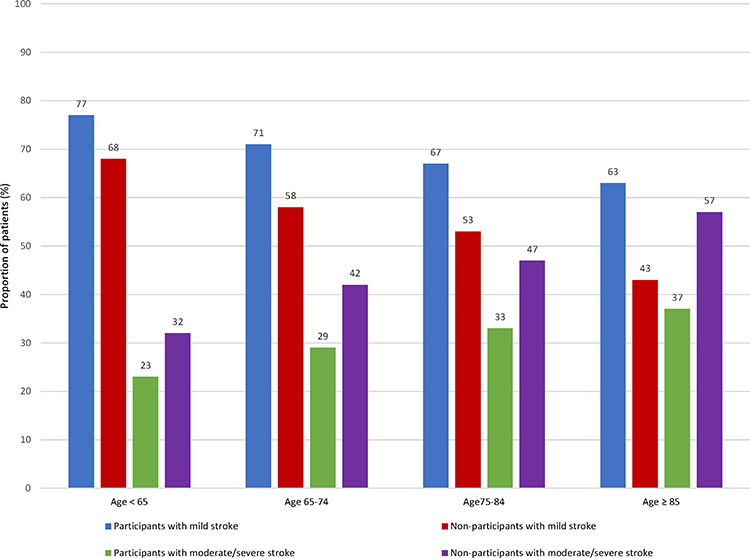 Purpose: The Norwegian Cognitive Impairment After Stroke (Nor-COAST) study aimed to estimate the prevalence and incidence of neurocognitive disorder in an unselected stroke cohort. The aim of the present study was to investigate whether selection bias occurred by comparing baseline characteristics from participants with non-participants in Nor-COAST.
Purpose: The Norwegian Cognitive Impairment After Stroke (Nor-COAST) study aimed to estimate the prevalence and incidence of neurocognitive disorder in an unselected stroke cohort. The aim of the present study was to investigate whether selection bias occurred by comparing baseline characteristics from participants with non-participants in Nor-COAST.
Patients and Methods: Nor-COAST is a prospective cohort multi-center study, recruiting participants from five Norwegian hospitals. Patients with the diagnosis of acute stroke were screened for inclusion. Baseline data from the participants recruited between May 2015 and March 2017 were compared to corresponding data from those not participating in Nor-COAST but registered in the Norwegian Stroke Registry. Regression analysis was used to assess whether age, stroke severity, sex and stroke subtype were independently associated with inclusion in the study.
Results: Out of 2505 available patients, 815 (32.5%) were included in Nor-COAST. There were no differences between participants and non-participants with respect to age (mean (SD) age 73.5 (11.7) versus 74.2 (14.5) years) or sex (44.8% versus 46.9% women). A significantly larger proportion of the participants were independent prior to stroke (87% versus 78%), had mild strokes (69% versus 55%) and suffered from cerebral infarction (90% versus 84%). The regression analysis showed decreased odds ratio (OR) of being included for those with higher degree of pre-stroke dependency (OR 0.895, 95% CI 0.825 to 0.971, p=0.007) and a more severe stroke (OR 0.952, 95% CI 0.939 to 0.966, p< 0.001).
Conclusion: The participants in Nor-COAST had a better pre-stroke health condition and milder strokes compared to non-participants. However, the participants should be regarded as representative of the majority of the stroke population which suffers from mild strokes. Nevertheless, baseline information for non-participants should be available also in future clinical studies to make it easier to identify which part of the stroke population the results can be generalized to.
Journal: Clinical Epidemiology
Published 1st of December 2020
Is long-bout sedentary behaviour assicated with long-term glucose levels 4 months after acute ischaemic stroke?
Is long-bout sedentary behaviour assicated with long-term glucose levels 4 months after acute ischaemic stroke?
Background: and purpose Sedentary behaviour is a risk factor for vascular disease and stroke patients are more sedentary than their age-matched peers. The association with glucose levels, as a potential mediator, is unclear, and we have investigated the association between long-bout sedentary behaviour and long-term glucose levels in stroke survivors.
Methods: This study uses data from the Norwegian Cognitive Impairment After Stroke study, a multicentre cohort study. The patients were recruited at hospital admission for acute stroke, and the follow-up was done at the outpatient clinic. Sedentary behaviour—being in a sitting or reclining position—was registered 3 months after stroke using position transition data from the body-worn sensor activPAL attached to the unaffected thigh. A MATLAB script was developed to extract activity data from 08:00 to 10:00 for 4 days and to categorise the data into four bout-length categories. The primary outcome was glycated haemoglobin (HbA1c), analysed at 3 months. Regression models were used to analyse the association between HbA1c and sedentary behaviour in the whole population and stratified based on a diagnosis of diabetes mellitus (DM). Age, body mass index and the use of antidiabetic drugs were added as covariates into the models.
Results: From a total of 815 included patients, 379 patients fulfilled the inclusion criteria for this study. We found no association between time in sedentary behaviour and HbA1c in the whole stroke population. We found time in sedentary behaviour in bouts of ≥90 min to be associated with a higher HbA1c in patients with DM.
Conclusion: Long-bout sedentary time is associated with a higher HbA1c in patients with DM 3 months after ischaemic stroke. Future research should investigate the benefit of breaking up sedentary time as a secondary preventive measure.
Journal: BMJ Open
Published 22nd September 2020
Vascular risk factor control and adherence to secondary preventive medication after ischemic stroke.
Vascular risk factor control and adherence to secondary preventive medication after ischemic stroke.
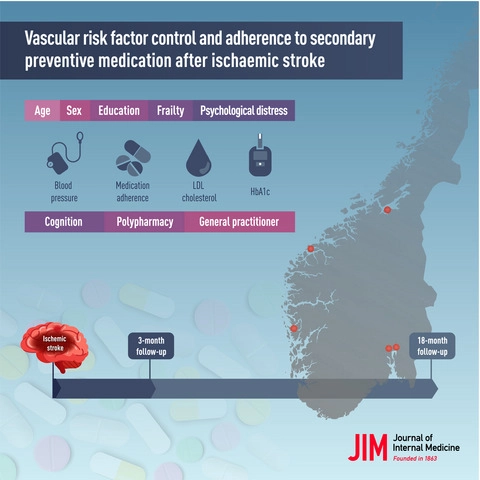 Background: Studies regarding adequacy of secondary stroke prevention are limited. We report medication adherence, risk factor control and factors influencing vascular risk profile following ischaemic stroke.
Background: Studies regarding adequacy of secondary stroke prevention are limited. We report medication adherence, risk factor control and factors influencing vascular risk profile following ischaemic stroke.
Methods: A total of 664 home-dwelling participants in the Norwegian Cognitive Impairment After Stroke study, a multicenter observational study, were evaluated 3 and 18 months poststroke. We assessed medication adherence by self-reporting (4-item Morisky Medication Adherence Scale) and medication persistence (defined as continuation of medication(s) prescribed at discharge), achievement of guideline-defined targets of blood pressure (BP) (<140/90 mmHg), low-density lipoprotein cholesterol (LDL-C) (<2.0 mmol L−1) and haemoglobin A1c (HbA1c) (≤53 mmol mol−1) and determinants of risk factor control.
Results: At discharge, 97% were prescribed antithrombotics, 88% lipid-lowering drugs, 68% antihypertensives and 12% antidiabetic drugs. Persistence of users declined to 99%, 88%, 93% and 95%, respectively, at 18 months. After 3 and 18 months, 80% and 73% reported high adherence. After 3 and 18 months, 40.7% and 47.0% gained BP control, 48.4% and 44.6% achieved LDL-C control, and 69.2% and 69.5% of diabetic patients achieved HbA1c control. Advanced age was associated with increased LDL-C control (OR 1.03, 95% CI 1.01 to 1.06) and reduced BP control (OR 0.98, 0.96 to 0.99). Women had poorer LDL-C control (OR 0.60, 0.37 to 0.98). Polypharmacy was associated with increased LDL-C control (OR 1.29, 1.18 to 1.41) and reduced HbA1c control (OR 0.76, 0.60 to 0.98).
Conclusion: Risk factor control is suboptimal despite high medication persistence and adherence. Improved understanding of this complex clinical setting is needed for optimization of secondary preventive strategies.
Journal: Journal of Internal Medicine
Published 2nd of August 2020
Post-stroke cognitive impairment – impact of follow-up time and stroke subtype on severity and cognitive profile.
Post-stroke cognitive impairment – impact of follow-up time and stroke subtype on severity and cognitive profile.
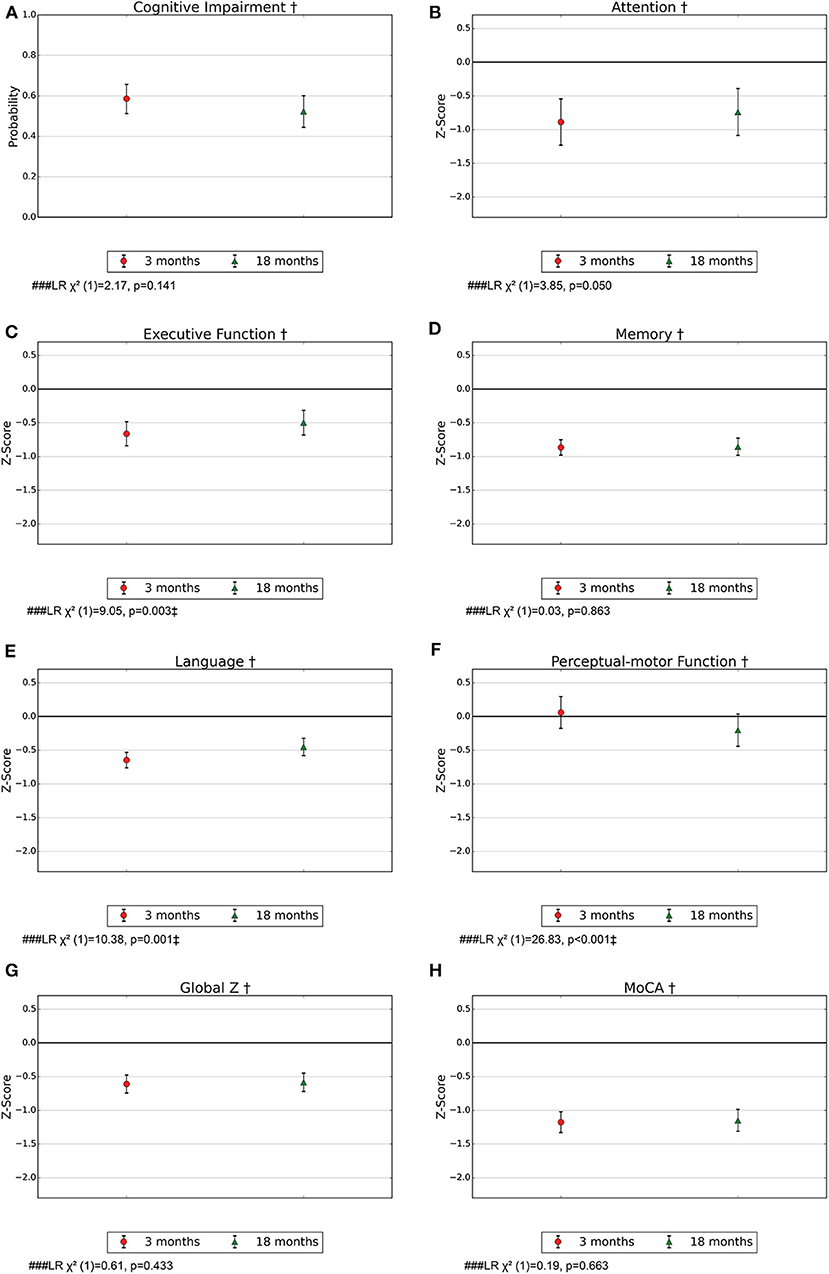 Background: Post-stroke cognitive impairment (PSCI) is common, but evidence of cognitive symptom profiles, course over time, and pathogenesis is scarce. We investigated the significance of time and etiologic stroke subtype for the probability of PSCI, severity, and cognitive profile.
Background: Post-stroke cognitive impairment (PSCI) is common, but evidence of cognitive symptom profiles, course over time, and pathogenesis is scarce. We investigated the significance of time and etiologic stroke subtype for the probability of PSCI, severity, and cognitive profile.
Methods: Stroke survivors (n = 617) underwent cognitive assessments of attention, executive function, memory, language, perceptual-motor function, and the Montreal Cognitive Assessment (MoCA) after 3 and/or 18 months. PSCI was classified according to DSM-5 criteria. Stroke severity was assessed with the National Institutes of Health Stroke Scale (NIHSS). Stroke subtype was categorized as intracerebral hemorrhage (ICH), large artery disease (LAD), cardioembolic stroke (CE), small vessel disease (SVD), or un-/other determined strokes (UD). Mixed-effects logistic or linear regression was applied with PSCI, MoCA, and z-scores of the cognitive domains as dependent variables. Independent variables were time as well as stroke subtype, time, and interaction between these. The analyses were adjusted for age, education, and sex. The effects of time and stroke subtype were analyzed by likelihood ratio tests (LR).
Results: Mean age was 72 years (SD 12), 42% were females, and mean NIHSS score at admittance was 3.8 (SD 4.8). Probability (95% CI) for PSCI after 3 and 18 months was 0.59 (0.51–0.66) and 0.51 (0.52–0.60), respectively and remained constant over time. Global measures and most cognitive domains were assessed as impaired for the entire stroke population and for most stroke subtypes. Executive function and language improved for the entire stroke population (LR) = 9.05, p = 0.003, and LR = 10.38, p = 0.001, respectively). After dividing the sample according to stroke subtypes, language improved for ICH patients (LR = 18.02, p = 0.003). No significant differences were found in the severity of impairment between stroke subtypes except for attention, which was impaired for LAD and CE in contrast to no impairment for SVD (LR = 56.58, p < 0.001).
Conclusions: In this study including mainly minor strokes, PSCI is common for all subtypes, both early and long-term after stroke, while executive function and language improve over time. The findings might contribute to personalizing follow-up and offer new insights into underlying mechanisms. Further research is needed on underlying mechanisms, PSCI prevention and treatment, and relevance for rehabilitation.
Journal: Frontiers neurology
Published 17th of July 2020
Impact of different methods of defining post-stroke neurocognitive disorder.
Impact of different methods of defining post-stroke neurocognitive disorder.
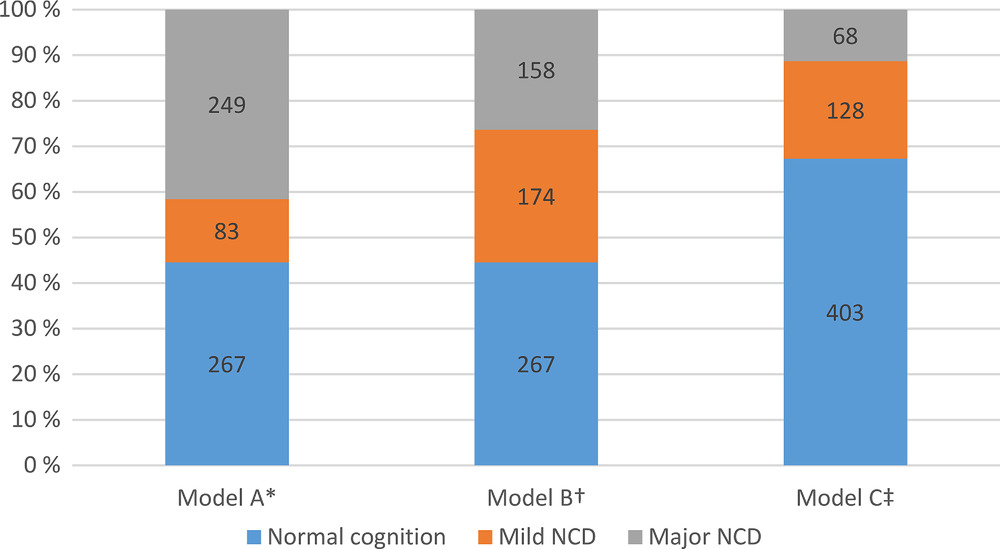 Introduction: Post-stroke neurocognitive disorder (NCD) is common; prevalence varies between studies, partially related to lack of consensus on how to identify cases. The aim was to compare the prevalence of post-stroke NCD using only cognitive assessment (model A), DSM-5 criteria (model B), and the Global Deterioration Scale (model C) and to determine agreement among the three models.
Introduction: Post-stroke neurocognitive disorder (NCD) is common; prevalence varies between studies, partially related to lack of consensus on how to identify cases. The aim was to compare the prevalence of post-stroke NCD using only cognitive assessment (model A), DSM-5 criteria (model B), and the Global Deterioration Scale (model C) and to determine agreement among the three models.
Methods: In the Norwegian Cognitive Impairment After Stroke study, 599 patients were assessed 3 months after suffering a stroke.
Results: The prevalence of mild NCD varied from 174 (29%) in model B to 83 (14%) in model C; prevalence of major NCD varied from 249 (42%) in model A to 68 (11%) in model C. Cohen's kappa and Cohen's quadratic weighted kappa showed fair to very good agreement among models; the poorest agreement was found for identification of mild NCD.
Discussion: The findings indicate a need for international harmonization to classify post-stroke NCD.
Impact of different methods of defining post-stroke neurocognitive disorder: The Nor-COAST study.
Journal: Alzheimer's Association
Published 16th of March 2020
Articles published in 2018
The Nor-COAST study: Study protocol of a multicentre, prospective cohort study.
The Nor-COAST study: Study protocol of a multicentre, prospective cohort study.
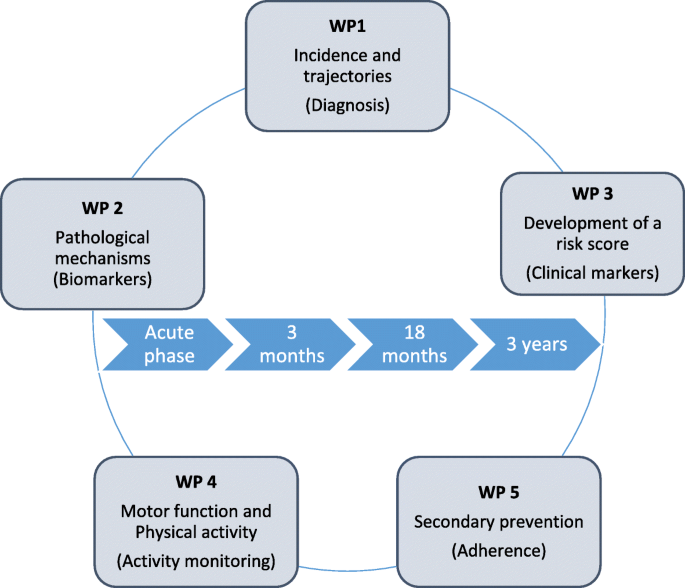 Background: Early and late onset post-stroke cognitive impairment (PCI) contributes substantially to disability following stroke, and is a high priority within stroke research. The aetiology for PCI is complex and related to the stroke itself, brain resilience, comorbid brain diseases, prestroke vulnerability and complications during the hospital stay. The aim of the Norwegian Cognitive Impairment After Stroke study (Nor-COAST) is to quantify and measure levels of cognitive impairments in a general Norwegian stroke population and to identify biological and clinical markers associated with prognosis for cognitive disorders following incident stroke. The study will be organised within five work packages: 1) Incidence and trajectories 2) Pathological mechanisms 3) Development of a risk score 4) Impact of physical activity and 5) Adherence to secondary prevention.
Background: Early and late onset post-stroke cognitive impairment (PCI) contributes substantially to disability following stroke, and is a high priority within stroke research. The aetiology for PCI is complex and related to the stroke itself, brain resilience, comorbid brain diseases, prestroke vulnerability and complications during the hospital stay. The aim of the Norwegian Cognitive Impairment After Stroke study (Nor-COAST) is to quantify and measure levels of cognitive impairments in a general Norwegian stroke population and to identify biological and clinical markers associated with prognosis for cognitive disorders following incident stroke. The study will be organised within five work packages: 1) Incidence and trajectories 2) Pathological mechanisms 3) Development of a risk score 4) Impact of physical activity and 5) Adherence to secondary prevention.
Methods: Nor-COAST is an ongoing multicentre (five participating hospitals), prospective, cohort study with consecutive inclusion during the acute phase and with follow-up at three and 18 months, and at three years. Inclusion criteria are stroke defined according to the WHO criteria. During the recruitment period from 18.05.2015 to 31.03.2017, 816 participants have been included. Cognitive impairment will be classified according to the DSM-5 criteria using a consensus group. Cognitive function is assessed by a standardised neuropsychological test battery, the Montreal Cognitive Assessment, Trail making A and B, ten-word immediate and delayed recall test, the Controlled Oral Word Association, Global Deterioration Scale and proxy based information by and the Ascertain Dementia 8 item informant questionnaire. Biomarkers include magnetic resonance imaging, routine blood samples and bio-banking. Clinical assessments include characteristics of the stroke, comorbidity, delirium, frailty and tests for cognitive and physical function, sensor based activity monitoring and adherence to secondary prophylaxis.
Discussion: Nor-COAST is the first Norwegian multicentre study to quantify burden of PCI that will provide reliable estimates in a general stroke population. A multidisciplinary approach aiming to identify biomarkers and clinical markers of overall prognosis will add new knowledge about risk profiles, including pre-stroke vulnerability and modifiable factors such as physical activity and secondary prophylaxis of relevance for clinical practice and later intervention studies.
Tidsskrift: BMC Neurology
Publisert 26 November 2018
Other publications
PhD-avhandling
Stina Aam (NTNU 2021). The Impact of Classification Models, Stroke Subtype, and Vascular Risk Factors on Courses of Poststroke Cognitive Impairment.
Forskerlinjeoppgave ved medisinstudiet
Marte Stine Einstad (NTNU 2019). Relationship between poststroke motor and cognitive impairment.
Masteroppgaver
Masteroppgave i Physical Activity and Health Geske Luzum (NTNU 2021). Physical activity behaviour, adherence to physical recommendations and associations with physical and cognitive function after stroke.
Masteroppgave i ergoterapi Live Øverlier (Oslo Met 2020). Fatigue hos slagpasienter i yrkesaktiv alder.
Masteroppgave i Human movement science Camilla Sollesnes Kummeneje (NTNU 2018). Sedentary behavior in individuals three months following stroke, and the association to physical function, cognitive function and mental health – The Nor-COAST study.
Masteroppgave i klinisk nevrologisk fysioterapi Torbjørn Sollie Johannessen (UiO 2018). Er det sammenheng mellom tester av kognitiv funksjon og balanse hos personer med akutt hjerneslag?
Masteroppgave i neuroscience Eva B. Aamodt (NTNU 2018). Examining the Characteristics of the participants Included in The Nor-COAST MRI sub study.
Masteroppgave i farmasi Ly Thi Ngoc Nguyen (NTNU 2017). Etterlevelse av anbefalt medikamentell sekundærprofylakse i en slagpopulasjon ved tre måneders oppfølging.
Hovedoppgaver medisinstudiet
Hovedoppgave medisin Kamilla Henny Giskegjerde og Ingunn Anette Halset (Universitetet i Bergen 2021). Sedentary behaviour during hospital stay in patients with acute stroke: A multicenter cohort study.
Hovedoppgave medisin Ingvill Svorkdal Sande (NTNU 2021). Kliniske kjennetegn av betydning for oppfølging hos fastlegen etter hjerneslag.
Hovedoppgave medisin Idunn Snorresdatter Wæhler (NTNU 2020). Relationship between In-Hospital Frailty and Quality of Life 3 and 18 months after a Cerebral Stroke: A prospective Cohort study.
Hovedoppgave medisin Kamilla Lind Helgheim (NTNU 2020). Secondary prevention follow-up after stroke in general practice – A substudy of the Norwegian Cognitive Impairment After Stroke (Nor-COAST) study.
Hovedoppgave medisin Marte Stine Einstad (NTNU 2018). Sub-classifying stroke of undetermined etiology- The Nor-COAST study.
Hovedoppgave medisin Karen Kuvås (NTNU 2018). The risk of selection bias in the Nor-COAST study. A case-control study.
Media articles
Nyhetsoppslag hos Helse Midt-Norge
Vil forbedre behandlingen av hjerneslagpasienter
Kognitiv svikt etter hjerneslag blir ofte oversett av helsevesenet, noe som rammer pasientene. Det vil forskerne bak Nor-COAST studien gjøre noe med.
Artikkel i Nasjonal Rapport fra Spesialhelsetjenesten 2020
Bedre behandling etter hjerneslag
Kognitiv svikt etter hjerneslag blir ofte oversett av helsevesenet, noe som får konsekvenser for pasientene. Det vil forskerne bak Nor-COAST-studien gjøre noe med.
Blogginnlegg på Forskning.no
MR-bilder av hjernen kan forutsi demens etter hjerneslag
Flere pasienter overlever hjerneslag på grunn av bedret behandling. Derfor lever flere pasienter og pårørende med konsekvensene etter en slik alvorlig hendelse. En fersk studie viser at MR-bilder av hjernen, allerede kort tid etter hjerneslaget, kan hjelpe oss å identifisere hvilke pasienter som står i faresonen for kognitiv svikt.
Artikkel på Forskning.no
Forskere kan forutsi mental svikt etter hjerneslag
Ved hjelp av MR-bilder kan de se at pasienter som utviklet kognitiv svikt, allerede hadde forandringer i hjernen før slaget.
List of scientific publications
2021
Alme, K.N., Ulvik, A., Askim, T. et al. Neopterin and kynurenic acid as predictors of stroke recurrence and mortality: a multicentre prospective cohort study on biomarkers of inflammation measured three months after ischemic stroke. BMC Neurology (2021)
Gynnild MN, Hageman S et al. Risk stratification in patients with ischemic stroke and residual cardiovascular risk with current secondary prevention. Akseptert for publikasjon i Clinical Epidemiology august 2021
Aamodt EB, Schellhorn T, Stage E, Sanjay AB, Logan PE, Svaldi DO, Apostolova LG, Saltvedt I, Beyer MK Predicting the Emergence of Major Neurocognitive Disorder Within Three Months After a Stroke. Front Aging Neuroscience (2021).
13:705889
Schellhorn T, Zucknick M, Askim T, Munthe-Kaas R, Ihle-Hanse H, Seljeseth, YM, Knapskog AB, Næss H, Ellekjær H, Thingstad P, Wyller TB, Saltvedt I, Beyer MK Pre-stroke cognitive impairment is associated with vascular imaging pathology: a prospective observational study. BMC Geriatrics (2021)
21:362
Aam S, Gynnild MN, Munthe-Kaas R, Saltvdt I, Lydersen S, Knapskog AB, Ihle-Hansen H, Ellekjær H, Eldholm RS, Fure B Impact of Vascular Risc Factors on Post-stroke Cognitive Impairments. The Nor-COAST study. Frontiers in Neurology (2021). 12:678794
Alme K, Askim T, Assmus J, Mollnes TE, Naik M, Næss H, Saltvedt I, Ueland PM, Ulvik A, Knapskog AB Investigating novel biomarkers of immune activation and modulation in the context of sedentary behaviour: a multicentre prospective ischemic stroke cohort study. BMC Neurology (2021) 21:318
Wæhler IS, Saltvedt I, Lydersen S, Fure B, Askim T, Einstad MS, Thingstad P Associaton between in-hospital frailty and health-related quality of life after stroke: the Nor-COAST study. BMC Neurology (2021) 21:100
Schellhorn T, Aamodt EB, Lydersen S, Aam S, Wyller TB, Saltvedt I, Beyer MK Clinically accessible neuroimaging predictors of poststroke neurocognitive disorder: a prospective observational study. BMC neurology (2021) 21:89
Einstad MS, Saltvedt I, Lydersen S, Ursin MH, Munthe-Kaas R, Ihle-Hansen H, Knapskog AB, Askim T, Beyer M, Næss H, Seljeseth YM, Ellekjær H, Thingstad P Associations between post-stroke motor and cognitive function: a cross-sectional study. BMC geriatrics (2021) 21:103
Munthe-Kaas R, Aam S, Saltvedt I, Wyller TB, Pendlebury ST, Lydersen S, Ihle-Hansen H Test Accuracy of the Montreal Cognitive Assessment in Screening for Early Poststroke Neurocognitive Disorder. Stroke.2021;52:00-00
2020
Kuvås KR, Saltvedt I, Aam S, Thingstad P, Ellekjær H, Askim T The Risk of Selection Bias in a Clinical Multi-Center Cohort Study. Results from the Norwegian Cognitive Impairment After Stroke (Nor-COAST) Study. Clin Epidemiology 2020:12 1327-1336.
Alme KN, Knapskog A-B, Næss H, Naik M, Beyer M, Ellekjær H, English C, Ihle Hansen H, Kummeneje CS, Munthe-Kaas R, Saltvedt I, Seljeseth Y, Tan X, Thingstad P, Askim Tbmc Is long-bout sedentary behaviour assicated with long-term glucose levels 4 months after acute ischaemic stroke? A prospective observational cohort study. BMJ Open 2020; 10:e037475
Gynnild MN, Aakerøy R, Spigset O, Askim T, Beyer MK, Ihle-Hansen H, Munthe-Kaas R, Knapskog AB, Lydersen S, Næss H, Røsstad TG, Seljeseth YM, Thingstad P, Saltvedt I, Ellekjær H Vascular risk factor control and adherence to secondary preventive medication after ischemic stroke. J Intern Med (2020)
Aam S, Einstad MS, Munthe-Kaas R, Lydersen S, Ihle-Hansen H, Knapskog AB, Ellekjær H, Seljeseth Y, Saltvedt I Post-stroke cognitive impairment – impact of follow-up time and stroke subtype on severity and cognitive profile in a minor stroke population: The Nor-COAST study. Frontiers neurology (2020)
Munthe-Kaas R, Aam S, Ihle-Hnasen H, Lydersen S, Knapskog AB, Wyller TB, Fure B, Thingstad P, Askim T, Beyer MK, Næss H, Seljeseth YM, Ellekjær H, Pendlebury ST, Saltvedt I Impact of different methods of defining post-stroke neurocognitive disorder: The Nor-COAST study. Alzheimers dement (2020) 6:e12000
2018
Thingstad P, Askim T, Beyer MK, Bråthen G, Ellekjær H, Ihle-Hansen H, Knapskog AB, Lydersen S, Munthe-Kaas R, Næss H, Pendlebury ST, Seljeseth YM, Saltvedt I. The Norwegian Cognitive Impairment after stroke study (Nor-COAST): study protocol of a multicentre, prospective cohort study. BMC Neurol. 2018 Nov 26;18(1):193
