Registry research for the health care services - Regforsk
Registry research for the healthcare services - Regforsk
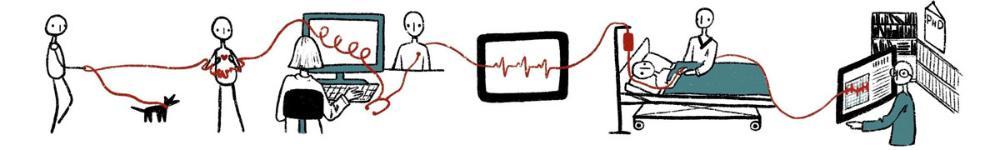
Regforsk is an interdisciplinary research environment that applies principles from randomized trials on registry data to study cause and effect in various treatments and the organization of healthcare services. Regforsk started as a project on capacity pressure in the health care services (2017-2025) and anchored through financial support from The Research Council of Norway (2019-2024). Regforsk aims to contribute with reliable scientific knowledge to support sustainable health services and strengthened public health.
Researchers widely consider randomized trials the gold standard for determining cause-and-effect relationships. Yet, randomizing changes at the system level has practical and ethical challenges. Healthcare research is therefore largely based on registered data from diverse sources, which in Norway is possible to link on an individual level. Such “real-life data” reflects the use of healthcare in daily practice over an extended period. Given certain assumptions, researchers can use linked registry data to study the effects of treatments and organizational structures.
Some examples of settings randomly assigning patients to doctors are out-of-hours services and allocation to general practitioners (GPs). In such cases, we can study doctors' preferred treatment and patients' further health outcomes as PhD candidate Schyler Marie Bennett explains with an example of mental healthcare. Another example is GPs retiring, which we assume they do independently of their patients. Thus, retirement can be considered a random event for patients, with effects on healthcare use and health outcomes.
Regforsk stems from NTNU and Trondheim University Hospital and consists of young and experienced researchers with backgrounds in epidemiology, various medical specialties, mathematics and statistics, social sciences, and health economics. Regforsk collaborates closely with several national and international researchers on a wide range of projects, both large and small. We are open to new collaborative opportunities.
Featured publications
Suicide and somatics
Suicide and somatics
We found heightened risk of suicide following discharge from acute somatic hospitalization, even in the absence of concurrent mental disorders, self-harm, or prior suicide attempts. This was particularly true for elderly individuals and underscores the need for support for patients after discharge.
What happens to patients when a GP quits?
What happens to patients when a GP quits?
We found that patients who experienced their general practitioner (GP) retiring or moving had a short-term, moderate increase in contact with out-of-hours GPs and acute hospital services, and a small but persistent increase in daytime GP and planned hospital contacts, compared to patients whose GP remained in the same practice. There was no difference in mortality between the patients.
Should out-of-hours doctors reduce their referral rates to hospitals?
Should out-of-hours doctors reduce their referral rates to hospitals?
We have studied the effects of referrals of elderly patients from out-of-hours services to hospitals in cases where the referral indication is not obvious - cases where some doctors would have chosen not to refer the patient. The study finds that such referrals lead to slightly more use of health services, but that those who are referred have significantly lower mortality over the next six months.
Hospital delivery volume, travel time, and birth outcomes
Hospital delivery volume, travel time, and birth outcomes
Location of maternity services involves balancing hospital delivery volume and travel time. It is not random which women give birth in smaller and larger hospitals. We therefore used three different research designs based on different assumptions to triangulate the results for birth outcomes:
1. We compared women who gave birth in hospitals of different sizes and with varying travel times, adjusted for known common underlying factors.
2. We compared women with themselves, if they moved between hospital areas between births.
3. We compared women who lived in neighboring municipalities, but in different hospital areas.
Triangulation showed opposite conclusions.
Overweight weighs more than obesity
Overweight weighs more than obesity
In the public debate, the focus is often on individuals with obesity and less at the population's BMI development. But what affects healthcare costs the most?
We found that people with severe obesity have a high individual risk of healthcare use, but they are few and affect total health care costs to a lesser extent than the much larger number of people with obesity.
This research shows that it is important to consider both the individual and population perspectives when evaluating measures against overweight and obesity, in clinical and health policy decisions, much in line with G. Rose’s discussion in Sick individuals and sick populations, in 1985.
Article in Tidsskriftet, The Journal of the Norwegian Medical Association.
Lectures and presentations from Regforsk
- Delayed nursing home admission
- Better off at home? Effects of nursing home eligibility
- Seminar on precision medicine
- Negative controls and causal inference
- Non-linear Mendelian randomization
- Causal inference course
- Estimation using instrumental variables
- The principles of instrumental variable analysis
- Introduction to causal inference
Funding



