Publications - CERG

Research results from CERG
Read the results from our publications.
Studies published in 2023
- Does resting heart rate affect the risk of atrial fibrillation?
- The Fitness Calculator reveals risk of aortic valve surgery
- Do genetics contribute to the health benefits in physically active?
- What do our fitness genes say about disease risk?
- Exercised blood stimulates to brain cell formation in rats with Alzheimers disease
- Patients with heart failure are able to attend digital exercise sessions
- Endurance athletes live longer
- Micro-RNA 133b is linked to more vulnerable coronary plaques
- Could subfractions of lipoproteins reveal future heart attacks?
- What does lipids in blood tell us about the lipid content of coronary plaques?
- Measuring fitness can give more precise cardiac diagnostics
- Exercise did not improve blood vessel function in heart failure
- More research needed to establish fitness genes and their impact on health
- The older you are, the faster your fitness declines
- Moderate exercise may be better for older adults' brain health
Studies published in 2022
- 4x4 interval training reduced atherosclerosis in heart patients
- 4x4 interval training improves health in common liver disease
- Improved fitness and activity levels following obesity rehabilitation
- Low stroke risk among veteran endurance athletes
- 100 PAI links to lower risk of a heart attack
- Interval training changes gene expression in the heart of smoke-exposed mice
- Identified a gene that affects both fitness and body weight
- Interval training in heart failure led to muscular changes that can improve fitness
- One in four covid-19 patients still have reduced physical capacity after one year
- Does etiology influence exercise response in heart failure?
- Coud Calanus oil supplementation increase physical fitness?
- PAI could be a great tool against dementia
- Does change in fitness affect medication for mental health issues in the elderly?
- How does exercise intensity affect signal conduction in the brain of the elderly?
- Interval training for heart failure patients improves the function of HDL particles
- Does kidney function influence exercise response in heart failure?
- Does hard exercise temporarily impair heart function more in persons with diabetes?
- Does interval training reduce vulnerable plaques in coronary arteries?
- New fitness genes found in record-breaking analysis
- High fitness can protect the elderly from structural brain impairments
- The higher cardiorespiratory fitness, the lower is the risk of heart surgery
- Micro-RNA and plaque burden change in interaction after exercise
- Impaired heart function is more common following severe covid-19 disease
- Low fitness is linked to adverse lipid profile
- Organized exercise dit not reduce progressive of white spots in older adults' brains
- Can blood plasma from fit donors help us treat Alzheimers disease?
Studies published in 2021
- Can gene therapy counteract muscle-wasting in the elderly?
- Can exercice reduce the risk of mild cognitive impairments among older adults?
- PAI is a useful activity standard for the whole world
- Does increasing fitness improve cognitive abilities in older adults?
- Does interval training lower cardiovascular risk more in older adults?
- Older men improved HDL cholesterol with interval training
- Blood test can reveal exercise response in heart failure
- What are the main reasons for impaired fitness after covid-19?
- Can exercise attenuate loss of brain volume in older adults?
- Walk test provides useful information on fitness after stroke
- Does hard exercise increase atrial fibrillation risk via effects on the immune system?
- How does high-intensity training impact walking and balance following stroke?
- Could carbohydrates make you run faster and longer?
- Does lung function impact cardiorespiratory fitness in COPD?
- Can your genes predict how you will respond to endurance training?
- Increased muscle-degrading activity in heart failure
- Has uncovered important mechanism for exercise response
- Could you exercise hard following pulmonary embolism?
- 70-year-olds with good fitness have higher blood volume
- Moderate exercise might benefit stiff, failing hearts the most
- Is high-intensity training harmful to failing hearts?
- Can 100 PAI prevent excessive weight gain?
- How does cardiorespiratory fitness impact life expectancy in people with arthritis?
- How should patients with diastolic heart failure exercise?
- Do women with heart disease benefit as much as men from high-intensity interval training?
Studies published in 2020
- Lives several years longer when PAI score is kept above 100
- Faster age-related decline in fitness among people with rheumatoid arthritis
- Does exercise make older adults live longer?
- Fitness declines less with age in active persons
- Interval training strengthens several functions in failing hearts
- Who are most physically active: Norwegian or Brazilian older adults?
- Knowledge from exercise can lead to new heart drugs
- Also Americans live longer with 100 PAI
- Could 4x4 interval training after a heart attack improve cardiac filling?
- Is exercise good medicine for cancer patients?
- Does lung function affect fitness in heart patients?
- What do we know about high-intensity interval training and youths?
- What do we know about high-intensity interval training and brain health?
- Exercise could reduce coronary artery plaques following stent implantation
- Is 4x4-minute interval training beneficial after a stroke?
- Persons with atrial fibrillation benefit from exercise and high fitness
- New fitness genes link to cardiovascular health
- Fitness predicts atrial size
- New Fitness Calculator for rheumatoid arthritis
Studies published in 2019
- What is the average fitness level of healthy men and women?
- How much does maximum stroke volume decrease with age?
- Lower exercise response in older and severely ill patients with heart failure
- Low fitness is an independent risk factor for dementia and death from dementia
- Change in high-energy phosphates is not suited to evaluate exercise effects in heart failure
- Miniscule molecules in blood could reveal heart attack risk
- Reduced risk of atrial fibrillation with high fitness
- Is weight gain harmful for the physically active?
- Reduced fitness in rheumatoid arthritis
- Does high fitness prevent myocardial infarction in both men and women?
- Is exercise-induced rhabdomyolysis normally dangerous?
- Regular runners have optimal lower body mitochondrial function
- Links poor fitness to increased inflammation
- High-intensity training restores myocardial mitochondrial function in diabetic mice
- Higher fitness linked to higher brain volume
- Exercise affects skeletal muscle metabolism in rats with heart failure
- Could exercise help oss develop new drugs against heart failure?
- How could exercise prevent and treat Alzheimer's disease?
- 100 PAI seems to secure high age-specific fitness
- Poor fitness predicts early death in non-alcoholic fatty liver disease
- Could skiers double pole to better fitness?
- What kind of exercise is most likely to increase fitness?
- Lung function could affect the physical capacity in healthy persons
- How can high fitness protect against metabolic diseases?
- Could a litte exercise improve skeletal muscle metabolism?
- Also healthy people avoid heart attacks by staying fit
- Is the maximum heart rate higher with lower fitness?
- Motivational interviewing helps stroke patients maintain physical activity
- 4x4 intervals improve fitness and body composition in psoriasis arthritis
- Increased risk of dementia in physically inactive persons with high psychological distress
- Lived longer after increasing the PAI score
- What kind of exercise does older adults prefer?
- Can exercise restore normal muscle function in heart failure?
- Also heart patients with 100 PAI live longer
- Should individuals with atrial fibrillation exercise?
- Which older adults are more likely to drop out of an exercise program?
- Does weather influence physical activity in the elderly?
- Can physical activity prevent atrial fibrillation?
- Can exercise prevent newborns' cardiac dysfunction following obese pregnancies?
- Exercise is linked to less dementia-related death
- How to exercise with peripheral artery disease
- The fit and happy live longer
- Heart patients live longer if they stay physically active over time
- Heart failure: Higher increase in oxygen uptake following high intensity interval training
- Effective high intensity interval training in obese children
- Rats escaped atrial fibrillation following high intensity interval training
- Should heart patients exercise the day before surgery?
- Obese children strengthen week hearts by exercising
- Why do failing hearts struggle during strenous acitivty?
The lower the resting heart rate one is genetically predisposed to have, the higher is the risk of getting atrial fibrillation. Low genetic resting heart rate is inherited randomly and thus not influenced by lifestyle and environmental factors that can change the resting heart rate. Thus, we can say with considerable certainty that it is a low resting heart rate in itself that increases the risk of future atrial fibrillation.
Previous studies have confirmed 46 genetic variants that are linked to a low resting heart rate, and these were the starting point for our analyses. In the study, we have examined genes and other health data in almost 70,000 women and men who participated in the Nord-Trøndelag Health Study between 1995 and 2008. We have also carried out the same investigations with data from the UK Biobank, where over 430,000 Britons contributed between 2006 and 2010.
By 2016, around 7,000 people from Trondheim had been confirmed to have atrial fibrillation, while more than 20,000 Britons had atrial fibrillation by 2021. Those who were genetically predisposed to the lowest resting heart rate had the highest risk. For each beat higher resting heart rate, the risk decreased by 4–5%. Very few people were genetically predisposed to a higher resting heart rate than 90, so we cannot say whether the risk of atrial fibrillation continues to decrease even with resting pulse values above 90.
Although a high resting heart rate in itself seems to protect against atrial fibrillation, it is not those with the highest resting heart rate in the population who have the lowest risk of getting atrial fibrillation. Both resting heart rate and risk of atrial fibrillation are affected by how we live, for example via blood pressure, BMI, smoking habits and level of physical activity. If one studies the link between resting heart rate and atrial fibrillation without taking these factors into account, it is those who have a resting heart rate between 60 and 80 - measured while sitting during the day - who have the lowest probability of getting atrial fibrillation.
The better the estimated cardiorespiratory fitness, the lower the risk of having to undergo aortic valve surgery. Aortic valve surgery is carried out in severe aortic stenosis, where the aortic valve is calcified and narrow and needs to be replaced. The study also shows that those who have undergone aortic valve replacement live longer if they have high fitness to begin with.
The study includes 57,214 men and women who participated in the Nord-Trøndelag Health Study in the mid-1990s (HUNT2) and/or in 2006–2008 (HUNT3). By 2018, 102 went through aortic valve surgery, and 35 of these died by April 2020.
We used the Fitness Calculator to estimate the fitness level of the participants. For every increase of 1 MET the risk of surgery was 15% lower. The 20% who had the highest estimated fitness for their age had more than halved the risk, compared to the 20% with the lowest fitness. The risk of early death after aortic valve surgery was 37% lower per 1 MET increase in estimated fitness level.
Genes that increase the likelihood to be physically active are also linked to a healthier health profile. Specifically, we found that the risks of stroke, high blood pressure and type 2 diabetes are lower the better activity genes you have. In addition, we linked better activity genes to healthier waist circumference, BMI and HDL cholesterol. Among other things, the analyzes were adjusted for self-reported level of physical activity among the study participants. Thus, the results may indicate that some of the health benefits in physically active people are genetic - and not caused by the physical activity itself. Nevertheless, the effect sizes were low for all the associations, and it is uncertain if the findings have any clinical significance. Further, we found no correlation between having good activity genes and directly measured cardiorespiratory fitness levels.
The study, which has been carried out in collaboration with Finnish researchers, uses data on genes, physical activity and risk factors from nearly 50,000 people who participated in the Nord-Trøndelag Helath Study (HUNT) between 2006 and 2008. All participants were given an overall score based on a number of gene variants that have previously been shown to be important for physical activity levels. We then investigated how this score relates to a number of health variables today and the risk of developing disease up to ten years in the future. There is some uncertainty linked to the findings, partly because the genetic activity score did not explain particularly much of the actual physical activity level of the participants in HUNT.
Genes that are linked to high fitness can also be linked to other things that affect our health. For example, our findings suggest that fitness genes also have an effect on the levels of creatinine in the blood and the risk of developing type 1 diabetes. We also found less certain signs that good fitness genes can lead to lower BMI, healthier levels of HDL cholesterol and lower resting heart rate.
We previously published the world's largest analysis of gene variants associated with directly measured fitness. In the new study, we investigated whether the 22 gene variants that were most closely linked to maximum oxygen uptake in that study are also linked to other measures of health. 65,000 participants from the second and third round of the Nord-Trøndelag Health Study have contributed data to the analyses. In addition to data from the health survey itself, we have also obtained information about hospital-registered diagnoses for the same people between 1999 and 2017.
Three of the gene variants that are linked to good fitness could also be linked to increased levels of creatinine in the blood. Increased levels of creatinine are associated with increased muscle mass. We can speculate that these three gene variants have an effect on muscle mass and in that way both give increased levels of creatinine and higher VO2 max. We checked the findings by doing the same analyses in a large British database, and found that two of the same gene variants were linked to increased creatinine levels. The analyzes from HUNT further indicate that a gene variant that increases fitness can significantly increase the risk of type 1 diabetes with neurological manifestations.
When we examined 33 gene variants that are only associated with fitness in men, we found that four of them are also linked to a significantly increased risk of endocarditis, an inflammatory disease of the inside of the heart. It is not unusual for genes linked to good health in one area to be bad for health in one or more other areas. For women, we found no reliable relationships between 44 gene variants and other health variables.
Although we did not find many reliable connections, we did make several interesting findings that have lower statistical power. Among other things, we saw signs that some of the genes that can give high fitness can also give a lower BMI for both sexes and healthier levels of HDL cholesterol and a lower resting heart rate for women.
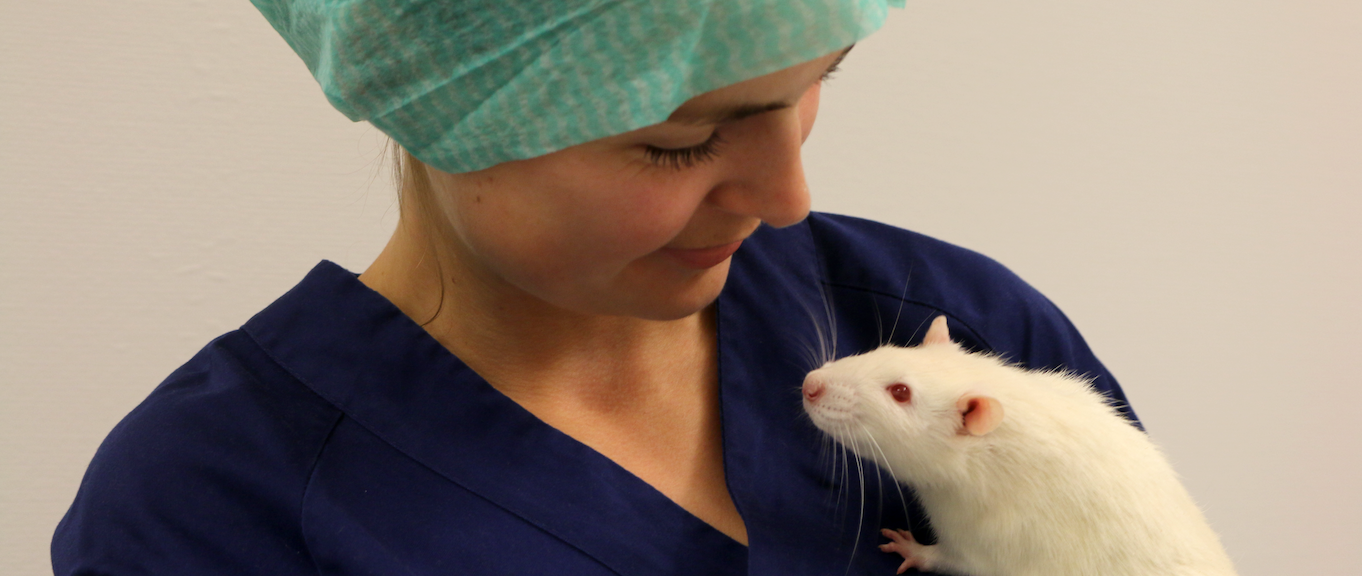
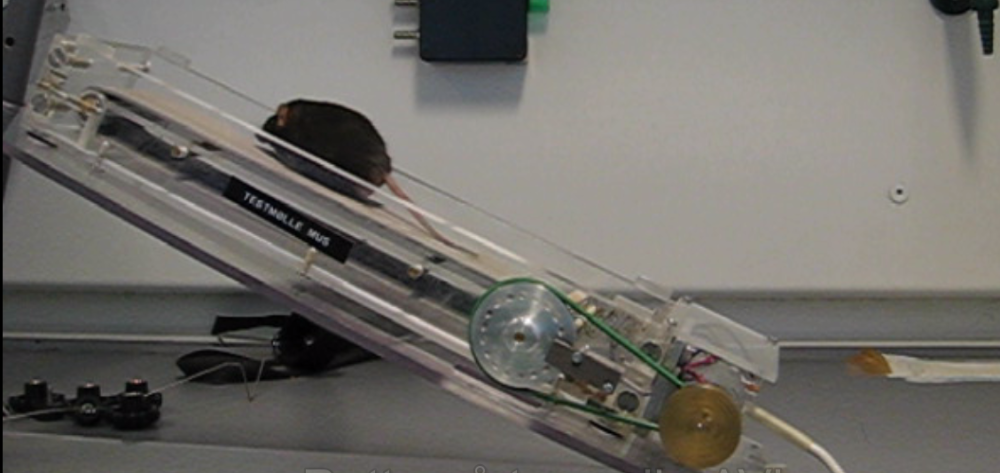
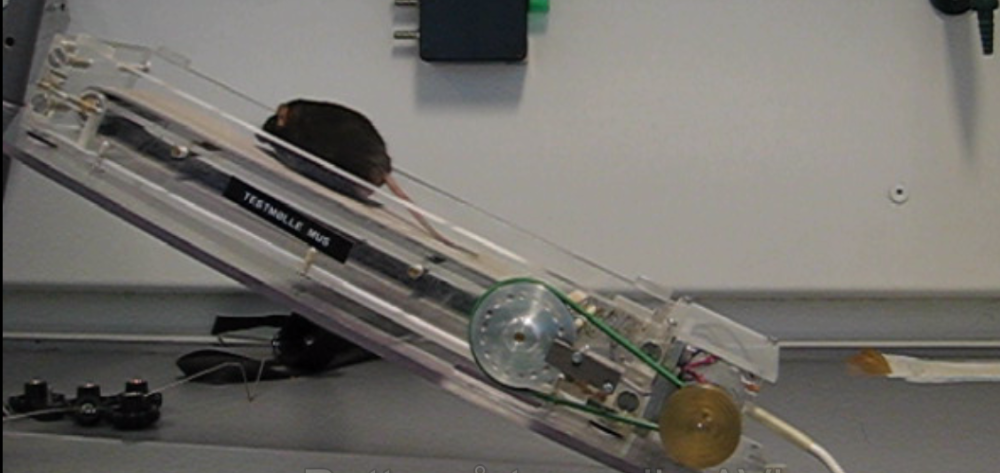
Blood plasma from men who have recently exercised counteracts impairments in Alzheimer's-like brain cells of mice. The brain cells from the mice were exposed to amyloid-β to simulate the damaged caused by Alzheimer's disease. Subsequently, the cell cultures were treated with plasma from endurance-trained men who had provided blood samples both before, immediately after, and up to one day after an intense workout. It turned out that the exercised blood prevented the mouse brain cells from shrinking in size and led to a higher proportion of healthy brain cells. This effect was most pronounced in the blood collected three hours after the exercise session.
We also transferred blood from rats that had performed six weeks of high-intensity interval training to rats genetically modified to develop symptoms of Alzheimer's disease. The rats received a total of 14 injections of exercised blood over six weeks. The rats that received the exercised plasma showed over a threefold increase in the formation of new brain cells in the hippocampus, compared to rats injected with saline solution. The hippocampus is a part of the brain important for short-term memory and learning, among other functions. This effect applied to rats that had not yet developed symptoms of Alzheimer's disease, as well as rats in a later stage of the disease.
Reduced inflammation could possibly be part of the explanation why exercised blood contributes to better brain health. The interval training led to lower levels of seven inflammation-inducing cytokines in the blood. Despite the increased formation of brain cells in the hippocampus, the injections with exercised plasma did not improve the rats' cognitive abilities. Trained plasma also did not reduce Alzheimer's-related plaques in the brain.
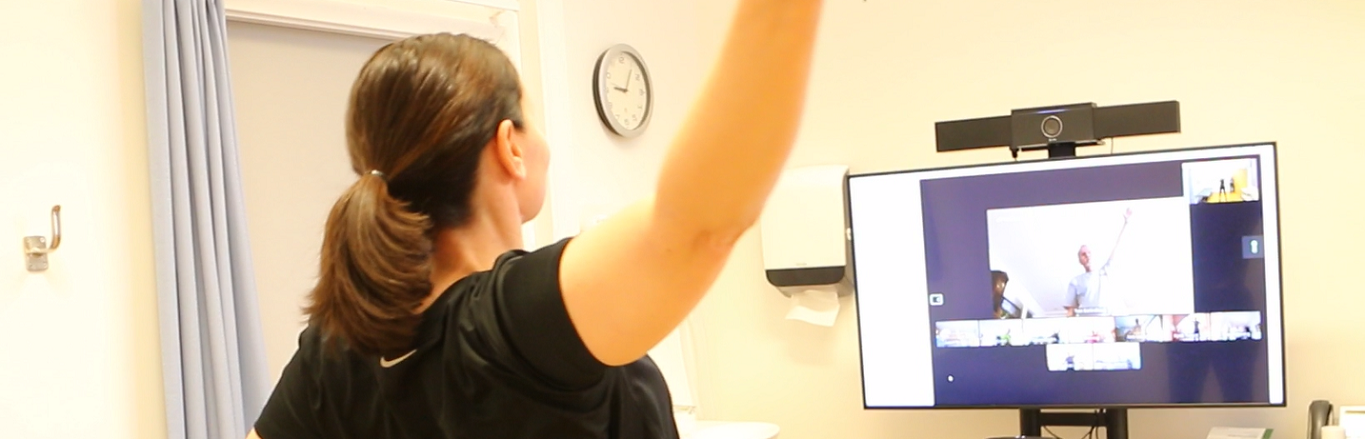
80% of heart failure patients who were offered home-based telerehabilitation participated in most of the exercise sessions. No one got sick or injured during the sessions, and almost all reported that they felt safe and wanted to continue exercising after the period of digital exercise follow-up ended. The results show that it is entirely possible for elderly patients with heart failure to take part in live exercise sessions with a physiotherapist via video link.
61 patients with heart failure participated in the study. The participants did not have the opportunity or desire to participate in the exercise groups at the hospital, but wanted to try home-based exercise. All attended a two-day course on how to live as well as possible with heart failure, but only half were given a tablet and offered to join digital exercise sessions directly from their own living room. Two days each week they could do intensive interval training via video transmission together with a physiotherapist, and the goal for everyone was to achieve 24 sessions.
The training was performed according to the 4x4 principle, with a focus on exercises for large muscle groups – for example, deep squats and fast walking or running on the spot.
Around 40% of the participants reached 24 sessions within four months, while another 40% took a slightly longer period to reach their goal. We also encouraged the participants to be active outside of the live exercise sessions. Among other things, they had access to pre-recorded exercise sessions on their tablet. They were asked to use these resources even after the period of supervised video exercise was over.
After the training period, the participants in the exercise group had improved by an average of 19 meters on a six minute walk test, but the control group improved by about the same amount. After another three months, we measured their maximum oxygen uptake. The participants in the training group had the same level of fitness as when the study started, while the control group had a significantly worse level of fitness. However, the difference between the groups was not statistically significant.
Thus, we can state that home-based telerehabilitation is feasible for patients with chronic heart failure. Our study also gives no indication that such training is not safe. However, the results cannot yet confirm that it is also more effective in improving physical fitness, compared to regular follow-up.
 Veteran cross-country skiers live longer than other physically active men
Veteran cross-country skiers live longer than other physically active men

Older men who engage in endurance sports competitions have a significantly increased chance of surviving the next ten years - even when compared to physically active men who do not participate in sports competitions. The findings may indicate that many years of active exercise and competition provide additional health benefits compared to training in line with the authorities' minimum recommendations.
In total, the study includes data from 2,370 men older than 65 years. 503 of them took part in the Birkebeiner cross-country ski race in 2009 and 2010 and were defined as athletes, while the other 2,757 took part in the Tromsø 6 survey between 2007 and 2008. After ten years of follow-up, 7% of the athletes had died, compared to 32% of the men from Tromsø. After taking into account that the athletes on average both had a higher education, smoked less and drank less alcohol, the risk of early death was still 66% lower than for the Tromsø men. Even lower BMI, medication use or the occurrence of diabetes and heart attacks could not explain the reduced mortality among the athletes.
In further analyses, we saw that the risk of early death was highest among the Tromsø men who reported being physically inactive. But we also saw that the men from the Birkebeiner race had roughly halved the risk compared to participants from Tromsø who reported a similar level of physical activity. The Tromsø participants who reported the highest level of physical activity had 57% lower risk of early death compared to those who were inactive, whereas the risk reduction among the the cross-country skiers who exercised the most was 79% .
The study is part of the NEXAF initiative, where our researchers collaborate with researchers from Bærum Hospital and the University of Tromsø.
Micro-RNA in the blood can reveal dangerous plaque in heart patients

The more fatty plaques the heart patients had in their coronary arteries, the higher were the levels of micro-RNA 133b in their blood. Thus, a blood test that analyzes this micromolecule can possibly help us to identify which patients are at high risk of having plaques that are likely to rupture and cause a heart attack.
Micro-RNAs are tiny molecules that regulate the activity of our genes. There are several thousand such micromolecules, and in our study we measured the levels of 160 different micro-RNAs in 47 patients with stable coronary artery disease. We also took ultrasound images of the inside of the patients' coronary arteries, and with the method of near-infrared spectroscopy we found the most fatty plaques.
Of all the microRNAs we examined, it was microRNA 133b that was most closely linked to plaque lipid content. The correlation was not weakened when we adjusted for traditional risk factors for cardiovascular disease. This suggests that micro-RNA 133b itself can reveal fatty plaques, but the strength of the association was moderate, and larger studies are needed to provide firm conclusions.
Among middle-aged and elderly people with a low risk of heart attack, we found no definite relationship between the levels of 112 different lipoprotein particles and future heart attack. In addition to looking at the total levels of, for example, LDL and HDL cholesterol in the blood, we divided these classic lipoproteins into groups based on size, density and concentration of lipids in the lipoprotein particles. Thus, we had the opportunity to look at whether, for example, small and dense HDL and LDL particles with a high concentration of cholesterol and other fatty substances were differently associated with heart attack risk than larger and less dense particles with a low fat content.
The study includes 50 people who had a heart attack within five years despite being healthy and having few or none of the classic risk factors when they participated in the third health survey in Nord-Trøndelag between 2006 and 2008. We compared them with 100 participants who did not have a heart attack within ten years but otherwise were similar to the participants who had a heart attack.
The main analyzes showed no clear connection between any of the 112 subfractions of lipoproteins and the risk of having a heart attack. In less rigid analyses, we found a connection between a high concentration of apolipoprotein A1 in the smallest HDL particles and an increased risk of future heart attack. For men, a low concentration of several lipids in large HDL particles was also linked to an increased heart attack risk. So, although we did not make any definite findings, the results provide a basis for looking more closely at whether subfractions of HDL particles can give us useful information about who is at increased risk of suffering a heart attack.
Lipid levels provide limited information on plaque content in heart patients

Using advanced analyses, we found two types of lipid particles that can potentially tell us something about the lipid content of plaque in patients with stable coronary artery disease. The patients with increased levels of lipoprotein(a) in the blood had, on average, slightly more fatty plaques in the heart's coronary arteries than patients with normal lipoprotein(a) levels. In addition, higher levels of free cholesterol in the smallest HDL particles were also associated to some extent with increased plaque lipid content. The two fatty substances did not, however, give us additional information about the plaque content beyond what we got by measuring traditional risk factors for cardiovascular disease.
Fatty plaques are more unstable than plaques with less fat, and thus increases the risk of a heart attack. However, it is difficult to measure the plaque content in the coronary arteries accurately, and it would be very useful to find biomarkers in the blood that can tell whether the calcifications contain much or little fat.
In the study, we examined the levels of 114 different lipoprotein groups in 56 patients with stable coronary artery disease. The analyzes does not only look at the levels of, for example, plain LDL and HDL cholesterol, but also the size, density and fat content of the various lipoprotein particles. The patients in the study underwent an advanced, invasive examination of the heart's coronary arteries, so that we could study the associations between the various fatty substances in the blood and the content of the most fatty plaques in the blood vessels of each patient.
With the traditional method for assessing heart size, nearly all elite athletes met the criteria for pathological left ventricular enlargement, while only 40% of heart failure patients did the same. However, when we took into account the maximum oxygen uptake (VO2 max) of the participants, the results were completely flipped: None of the elite athletes, but almost all of the patients, had enlarged hearts.
Exercise causes the heart chambers to grow in a healthy and balanced way, unlike pathological enlargement that occurs as a compensatory mechanism in weak hearts. At the same time, we know that larger individuals naturally have larger hearts. The usual method of assessing whether a person has normal heart size is to adjust ultrasound results based on the body surface area of the person. In other words, it takes into account that body size affects the structure of the heart, but not that exercise status also does. In our study, we compared this method to a method where, instead of indexing for body surface area, we indexed for the absolute VO2 max of the participants.
We used ultrasound and fitness measurements from 13 elite athletes and 58 endurance athletes, 1190 healthy men and women, and 61 patients with heart failure. The results from the healthy non-athlete participants were used as reference material for normal and enlarged left ventricular volume, and athletes and heart failure patients were classified based on these reference values.
Among the healthy participants, we found a significantly stronger correlation between VO2 max and left ventricular size than between body surface area and left ventricular size. Using the traditional method, only 24 heart failure patients were defined as having an enlarged left ventricle, while the number increased to 58 (95%) when we used the VO2 max method. For elite athletes, the number of individuals with an enlarged left ventricle dropped from 12 to 0 when we switched measurement methods. The diagnosis was also more accurate for the non-elite endurance athletes, with only one of the 58 having an enlarged left ventricular based on our new measurement criteria, compared to six out of 58 with the traditional method.
Fitness measured as absolute maximum oxygen uptake shows how many liters of oxygen a person can use for energy production each minute. Therefore, this measure takes into account both exercise status and body size. It is not surprising, then, that indexing for VO2 max provides a more precise indication of whether left ventricular size is normal. This new method may prevent the misclassification of healthy hearts as diseased, reducing the need for costly and unnecessary further investigation. There is also potential to use this method in the assessment and diagnosis of heart failure and other heart diseases.
The exercise in our large OptimEx study did not lead to better blood vessel function for the patients. Some patients with heart failure have damaged and dysfunctional blood vessels, and among 159 participants in OptimEx, we measured both the stiffness of large blood vessels, the ability of smaller vessels to dilate, and the function of endothelial cells that line the inside of the vessel wall, in the smallest blood vessels. 70% had impairments in one or more of these measurements, and about half also had reduced levels of cells that repair damaged blood vessel walls.
Neither the group that was assigned to perform 4x4-minute interval training, nor those who exercised with moderate intensity, achieved better blood vessel function during the exercise period. There were no improvements neither after three months of supervised exercise nor after an additional nine months of exercising at home. Furthermore, the levels of markers for repair of endothelial cells did not increase.
The participants in OptimEx have heart failure even though the pumping function of the heart is intact. The main article from the study showed that the exercise resulted in improved endurance capacity (maximum oxygen uptake), despite the fact that the heart did not become better at pumping blood. Since the exercise also did not improve oxygen delivery to the muscles through better blood vessel function, it appears that improved maximum oxygen uptake in this patient group is primarily due to the fact that exercise can improve the muscles' ability to take up oxygen from the blood and use this oxygen for energy production.
Our genes likely determine about half of our maximum oxygen uptake. Our genes also play a significant role in how physically active we are and how our bodies respond to exercise. However, even though we know that genetics are important, we still lack knowledge about which genes affect fitness, activity levels, and training response.
Our researchers have now summarized knowledge from the best and latest studies on genes related to maximum oxygen uptake, physical activity level, and exercise response. CERG have conducted the largest study to date looking for genetic variants associated with directly measured maximum oxygen uptake. We found several individual genes related to fitness, especially in women. Some larger studies have also identified genetic variants that appear to be related to physical activity level measured by activity monitors. However, research has not yet been able to uncover a single gene that can be confidently linked to training response.
The main challenge with these types of studies is that a large number of participants are needed to establish reliable relationships. Since so few fitness and activity genes have been identified so far, we currently know very little about the potential biological mechanisms that could explain why these genes have an impact. This is something our group wants to investigate further in upcoming studies.
We also want to know more about whether fitness and activity genes are also related to other risk factors for heart disease. There are studies suggesting that good fitness may be particularly important for people who have a high genetic risk of developing heart disease. We also assume that exercise and fitness affect the risk of lifestyle diseases by changing the behavior of our genes, known as epigenetics. However, more research is needed before we can provide reliable answers.
Maximum oxygen uptake drops faster as you get older. Based on studies that only measure fitness at one point in time, it has generally been calculated that the fitness number falls by 10% per decade, or by between 0.3 and 0.5 ml/kg/min per year. However, in the few large studies that have measured the fitness levels of the same people twice with several years in between, fitness numbers decline by up to 20% per decade for women and 25% for men aged over 70, while it declines by less than 10% per decade among young adults.
The results are described in a new review article in which our researchers considered all major population studies that have measured oxygen uptake at one or two points in time. The reason why we should rely more on data from studies with multiple measurements is that, to a greater extent, only the healthiest elderly, who are in good shape for their age, will take part in studies with single measurements. Thus, the average maximum oxygen uptake that is measured in the oldest age groups will probably be higher than the real average for the entire population.
Aging in itself, but also the fact that the level of physical activity tends to decrease as one gets older, are likely reasons why the fitness number drops faster with each decade as we get older.
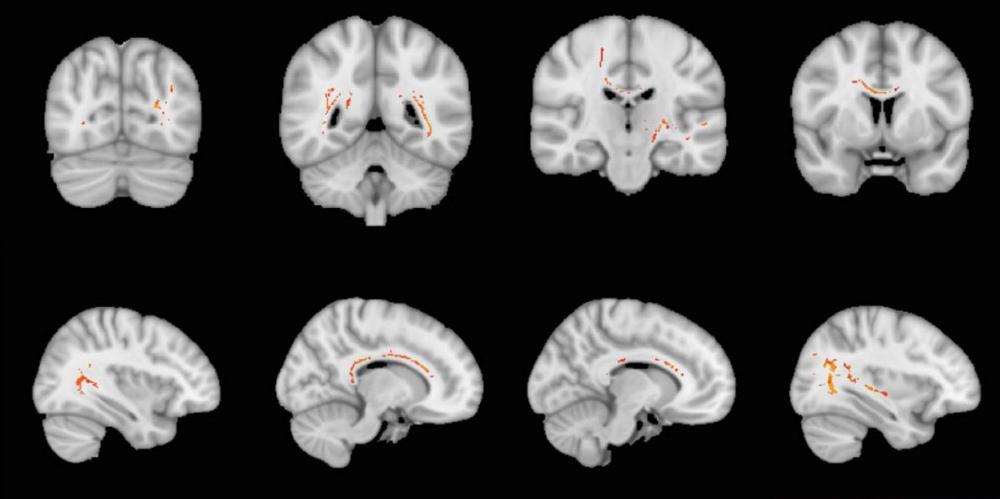
Avoiding very high-intensity exercise and following the health authorities' physical activity recommendations may be the most beneficial for the elderly in terms of keeping healthy brain cells in the hippocampus. After three years of exercise, it was the control group of the Generation 100 study that had the highest N-acetylaspartate:creatine ratio in the hippocampal body, whereas the choline:creatine ratio was lowest in the participants who reported to exercise most intensively.
The neurochemical N-acetylaspartate signals healthy neurons, while choline is important for the cell membranes of the nerve cells. The hippocampus is a part of the brain that, among other things, is important for our memory. However, the differences we found does not seem to have affected the cognitive function of the participants. On the contrary, it was actually the participants with the lowest choline:creatine levels in the hippocampal body who scored highest on the cognitive test.
In the anterior part of the hippocampus, we found no difference in the levels of neurochemicals, neither between the groups nor based on reported exercise intensity. We also investigated whether maximum oxygen uptake had an effect on the metabolites, but neither fitness level at the same time nor changes in fitness over time played any role.
In the Generation 100 study, men and women aged 70 to 77 were randomly allocated to organized exercise follow-up for five years, or to participate in the control group which were told to follow the authorities' recommendations for physical activity. This substudy includes analyzes from 63 of the participants, and we measured the levels of N-acetylaspartate, choline and creatine by performing MR spectroscopy after three years. Most of the participants exercised well throughout the period, and the participants in the control group to a high degree followed the recommendations to exercise with moderate intensity 30 minutes most days of the week.
Interval training can reduce atherosclerosis in heart patients

Regular high-intensity 4x4-minute interval training for six months reduced the amount of plaque in the coronary arteries of patients recently treated for stable angina. This is the first study that has been able to demonstrate that exercise can reduce residual atherosclerosis in patients following treatment for narrow coronary vessels.
The study includes 60 patients. They were randomly assigned to two groups. One half attended guided 4x4 interval training two days a week for six months. The other half received regular exercise advice without any offer of direct follow-up. Both before starting and after six months, we examined the atherosclerosis in the coronary arteries with ultrasound images taken from inside the coronary arteries.
After six months, the interval training had reduced the amount of plaque compared to the control group, where the amount of plaque was unchanged. The training also led to the participants increasing their maximum oxygen uptake by 10%, while reducing their waist measurement by five centimeters on average.
Both the amount of plaque in the heart's coronary arteries and the plaque composition play roles in the risk of having a heart attack. In a previous article, we have shown that the interval training apparently did not stabilize the plaques more than usual treatment, but that the participants who increased their fitness had more stable plaques.
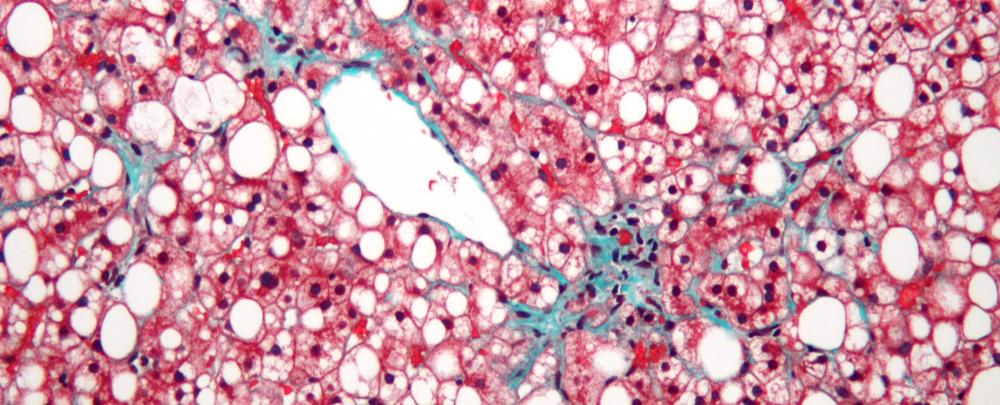
4x4 interval training improves physical capacity and insulin sensitivity in people with nonalcoholic steatohepatitis. This is a condition that is common among people with non-alcoholic fatty liver disease, and which involves signs of cell death, inflammation or an increased amount of connective tissue in the liver. In addition, most people with steatohepatitis are insulin resistant and obese.
The pilot study, which was conducted by Australian researchers – including our postdoctoral researcher Ilaria Croci – included 14 participants with non-alcoholic steatohepatitis. Eight were drawn to complete 4x4 intervals three days each week for 12 weeks. The last six instead met to carry out stretching exercises.
Surprisingly, those who did 4x4 intervals did not increase their maximal oxygen uptake. But on a cycling or walking/running test to exhaustion, they lasted on average two minutes longer than those who had only stretched. The training effect on insulin sensitivity and cholesterol levels was also large, and several areas within health-related quality of life improved.
The study also showed that 4x4 interval training is safe and feasible for this patient group. Furthermore, the interval training led to better liver fat values, lower BMI and reduced waist circumference, although these results were not statistically significant due to the small number of participants.
Both heart function, physical activity level, BMI and maximum oxygen uptake improved for people with severe obesity who participated in a multidisciplinary obesity rehabilitation program. 56 men and women with a high BMI joined the study, and within a year 38 of them completed three three-week stays at the Norwegian Heart and Lung Association rehabilitation clinic at Røros. After both six months and one year, they had lost close to 6 kg on average and also achieved several other health effects.
During their stay at Røros, the participants were followed up by a doctor, nutritionist, physiotherapist, occupational therapist and a nurse with expertise in cognitive behavioral therapy. They carried out a number of health talks and received, among other things, theoretical and practical introductions to physical activity.
Many people with severe obesity have hearts that relax poorly between each beat, which can eventually develop into heart failure. However, in this study, where the average age of the participants was as low as 44 years, only six of the participants had impairments so great that they were diagnosed with diastolic dysfunction. Still, after six months, several measures of heart function had improved in the group as a whole, both when it came to the heart's pumping power and ability to relax.
In addition, the average BMI was reduced from approximately 40.5 to 39 kg/m2, while the maximum oxygen uptake increased from 25 to 27 ml/kg/min. The participants had also become more physically active than they were at the start. Importantly, all the changes persisted at one year's follow-up.
Low risk of stroke among veteran cross-country skiers

Although the risk of atrial fibrillation is higher for long-term endurance athletes than for the general population, the risk of stroke is lower. Atrial fibrillation increases the risk of stroke, but the first results from the nationwide NEXAF project now show that older men who have taken part in the Birkebeiner ski race have about 40% lower risk of stroke than men from the general population.
However, the results also show that athletes with atrial fibrillation are more than twice as susceptible to stroke as athletes without atrial fibrillation. This increase in risk is still low compared to most men, where atrial fibrillation is linked to a fourfold risk of stroke.
The findings are based on data from more than 500 athletes from all over the country and close to 2,000 men of the same age from Tromsø. All the athletes were over 65 years old when they took part in Birkebeinerrennet in 2009–2010. On average, they had participated in 14 editions of the ski race. All answered a questionnaire about exercise, other lifestyle habits and history of diseases, and 88% answered similar forms again in 2014 and/or 2020. The 1,867 participants from Tromsø were also over 65 years old when they took part in the sixth edition of The Tromsø Study in 2007–2008, and just over half of them participated again in Tromsø 7 eight years later.
Almost 30% of the Birkebeiner athletes stated that they had atrial fibrillation, compared to just under 20% of the men from Tromsø. After taking into account that the athletes on average had far fewer risk factors for lifestyle diseases, lower BMI, higher level of education and healthier smoking and drinking habits, the risk of atrial fibrillation was increased by almost 90% compared to the Tromsø men. This difference is probably somewhat smaller in reality, as there was a higher proportion of athletes than general men who answered the follow-up questionnaires.
Regarding stroke, the incidence was 5% among athletes and 10% among the men from Tromsø. Athletes with atrial fibrillation also had a lower risk of stroke than non-athletes without atrial fibrillation. Overall, the results suggest that exercise-related atrial fibrillation entails a lower risk of stroke than atrial fibrillation caused by traditional cardiovascular risk factors.
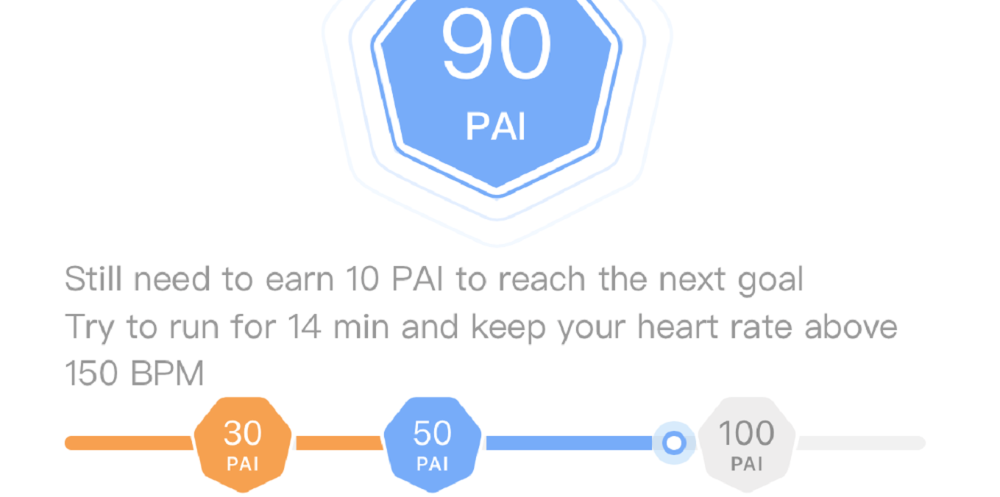
Older Chinese men and women who achieve a physical activity level of 100 PAI or higher have lower risk of a future heart attack than less active Chinese of the same age. The risk of dying from a heart attack or angina pectoris is also reduced for those who achieve 100 PAI, and this also applies to the middle-aged. The association between PAI and health risk apparently cannot be explained by other differences between active and inactive people, as the analyzes are adjusted for a number of such differences.
The study uses health information from close to 450,000 healthy men and women from ten different regions in China. Between 2004 and 2008, they reported their exercise habits and had a number of other health variables measured, such as blood pressure, BMI and blood sugar. 1,808 of the participants had a heart attack by 2015, while 3,050 died of a heart attack or angina. For people over 60 who achieved at least 100 weekly PAI, both the risk of having and dying from a heart attack was reduced by 16%. Also, among people with high blood pressure, diabetes and obesity, 100 PAI was linked to a lower risk of dying from a heart attack or angina.
Two specific changes in cardiac gene expression after high-intensity interval training might correct some of the damage that occurs in the heart when smoking. In a previous study, we showed that mice exposed to cigarette smoke had impaired heart function, but that six weeks of interval training almost reversed these impairments. We have now looked for genetic mechanisms that can explain these exercise effects.
It turned out that the expression of several genes in both the left and right heart chambers was different in the mice that had exercised, compared to the mice that were only exposed to smoking without exercise. Further investigations showed that two of the gene markers in the left ventricle - Agt and Retnla - are probably regulated by exercise in mice exposed to cigarette smoking. Smoking can damage DNA directly and also affect which RNA copies are made from the DNA. Similarly, exercise can change the expression of important genes. Based on the findings, we speculate that exercise-triggered changes in the Agt and Retnla genes may lead to better heart function and physical capacity in mice exposed to cigarette smoke.
The gene COX7A2L appears to be an important gene for physical capacity. Among other things, the gene affects the formation of important protein complexes in the mitochondria, which are the power plants of our cells. In the long term, the findings could potentially lead to new forms of treatment for lifestyle diseases, for example by changing the properties of this fitness gene in people who have a less favorable variant.
In the study, we used data from the HUNT3 Fitness study to confirm that the COX7A2 gene may be important for maximum oxygen uptake in humans. People with a genetic variant that gives increased levels of the RNA strand COX7A2L in skeletal muscle have higher maximum oxygen uptake than those who do not have this genetic variant. In addition, the study reveals, using data from other population studies, that the same favorable genetic variant can not only provide increased fitness, but also reduce body fat and body weight.
The study, which is a collaboration between researchers in Switzerland, Finland, Spain and CERG, shows that the composition of the COX7A2L gene is decisive for how many stable RNA copies the gene produces, especially in skeletal muscle cells. Ten letters in a specific part of the gene turned out to be the most important, Muscle fibers that have the "correct" letter composition in both pairs of this gene get increased levels of the RNA strand COX7A2L when the muscle cells are exposed to metabolic stress, such as exercise.
The energy that enables our muscles to move is produced in the mitochondria of muscle cells. The vast majority of energy production is dependent on oxygen, and takes place in the form of cellular respiration in four protein complexes inside the mitochondria. The protein complexes cooperate with each other in so-called supercomplexes, and mitochondria with well-functioning supercomplexes can thus play a role for oxygen uptake. The study shows that the COX7A2L gene plays an important role for these supercomplexes: Muscle fibers with the favorable genetic variant, which gives increased COX7A2L levels, also have more supercomplexes and an increased potential for cellular respiration in the mitochondria.
Finally, the study tested the effect of the fitness gene in a species of mice who are normally born without the Cox7a21 gene. Mice from the same species that were nevertheless bred to have this gene, had both increased maximum oxygen uptake, more muscle mass and increased energy consumption during physical activity. Furthermore, the results showed that exercise led to increased RNA levels of Cox7a2l in these mice, and that the exercise also produced more potent supercomplexes in the mitochondria.
Molecular changes in skeletal muscle may contribute to increased maximal oxygen uptake in patients with diastolic heart failure after a period of 4x4 interval training. This group of patients has hearts with normal pumping capacity, but which nevertheless beat weakly because they are unable to fill well with blood between each beat. Exercise seems to have a limited effect on the filling of the heart in these patients, and changes in the muscles can thus be directly decisive for achieving better fitness.
In a sub-study of the OptimEx study, we extracted muscle samples from some of the participants before starting, after three months of supervised exercise, and after a further nine months where they mostly were told to exercise on their own. We analyzed the gene expression of several proteins linked to muscle wasting and the activity of enzymes that are important for the metabolism in the muscle cells. Many patients with heart failure have a dysfunctional metabolism that can lead to reduced insulin sensitivity and muscle wasting. We also measured the quantity and function of satellite cells in the muscles. These are stem cells located outside the muscle fibres, but which after an exercise period can fuse with the muscle fibers and make them grow.
Both training with moderate intensity and interval training with high intensity gave the participants better fitness during the first three months, compared to the control group that did not participate in organized training. Moderate training only led to small molecular changes in the muscles. On the other hand, the high-intensity interval training influenced the metabolism in a favorable direction and also led to more satellite cells with better function. After twelve months, however, all the improvements had disappeared, which can probably be explained by the fact that fewer participants continued to follow the exercise plan after the face-to-face supervision ended.
Most people who have been hospitalized with covid-19 have normal cardiorespiratory fitness one year later. The majority also achieved a higher maximum oxygen uptake than they had three months after admission. Nevertheless, almost a quarter still have poorer fitness than is expected for their age, and their fitness is lower than that of otherwise similar people without a history of covid-19.
In the study, we measured the fitness of 210 men and women who had been admitted to hospital with severe coronavirus disease during the first months after the pandemic arrived in Norway. We then compared with reference values for maximum oxygen uptake among Norwegians. After three months, 34% of corona patients had at least 20% worse fitness than most of their peers, while this proportion had dropped to 23% after a year.
We have also investigated whether the fitness of the covid patients differs from the fitness of others with the same sex, age, BMI, blood pressure and comorbidities. In these analyses, we have compared with selected participants from the HUNT4 Fitness Project, which was carried out in the years before the covid-19 pandemic. It turned out that the covid-19 patients had, on average, lower cardiorepiratory fitness than the HUNT participants.
The study, which was carried out in collaboration with six Norwegian hospitals, also indicates that physical inactivity is the most important reason why oxygen uptake is still impaired in some people 12 months after severe coronavirus disease. Limitations of the airways were rarely the cause, while the heart and circulation limited fitness in some of the patients.
Exercise has the same effect for patients with heart failure, regardless of whether the disease has ischemic or non-ischemic origin. Myocardial infarction is the most common cause of ischemic heart failure, while long-term high blood pressure and valve disease are among the most common causes of non-ischemic heart failure, where the failing pumping function of the heart is not due to a lack of oxygen.
In the SMARTEX-HF study, over 200 patients from nine research centers in Europe were randomly drawn to three groups. The participants were either followed up with supervised high- or moderate-intensity exercise for 12 weeks, or were given advice to exercise on their own. For the following nine months, all the participants exercised by themselves.
In this substudy, we compared participants from all three groups based on whether they had heart failure of ischemic or non-ischemic ethiology. Neither three nor 12 months of exercise follow-up had a different effect on the heart's structure or pump function, nor did physical fitness change differently in the two patient groups.
Calanus oil has no effect on maximum oxygen uptake

Healthy men and women do not improve their cardiorespiratory fitness by taking supplements with Calanus oil, which is extracted from the copepod calanus finmarchicus and is rich in omega-3 fatty acids. Previous animal studies gave us a hypothesis that this oil could have an effect on the maximum oxygen uptake. But after half a year of daily supplementation, fitness had not increased in the participants who received Calanus oil, compared to those who received placebo. Both at the start of the study and after six months, the average fitness number in both groups was approximately 50 ml/kg/min.
The participants were randomly drawn to receive a supplement with 2 g of Calanus oil every day, or an equivalent amount of placebo. Neither the participants themselves nor we who tested them knew which oil they received. We did not give them specific instructions about physical activity. 58 people between the ages of 30 and 60 completed the six-month study, and we tested their fitness both before, three months into and immediately after the intervention.
People who maintained an activity level of 100 PAI over a ten-year period – and those who increased from below to at least 100 PAI during the period – had a significantly lower risk of developing dementia over the next 25 years, compared to those who were less physically active. The risk of dying from or with dementia was also reduced for those who exercised enough to achieve 100 PAI. On average, participants with at least 100 PAI lived almost three years longer without dementia than those who were less active.
PAI - Personal Activity Intelligence - is a unique standard for measuring physical activity, developed by us at CERG. We obtained the results for the new study by analyzing data on almost 30,000 women and men who were healthy when they participated in the Nord-Trøndelag Health Study in both the mid-1980s and 1990s. By using the Norwegian Cause of Death Registry and a local dementia register for the hospitals in Nord-Trøndelag, we found that just over 1,000 of the participants died of dementia by May 2020, while approximately 2,000 received a dementia diagnosis before February 2021.
The PAI score of the participants was calculated based on how active they reported to be when attending the two health surveys. Those who had a PAI of at least 100 in both the 1980s and 90s had a 38% lower risk of dying from or with dementia, compared to those who were physically inactive at both times. The risk of developing dementia was reduced by 25%. This reduction in risk applied after we had taken into account other differences between the active and inactive participants, for example that the inactive on average had higher blood pressure, smoked and weighed more, had lower education and more often lived alone.
We also saw an almost similar reduction in dementia risk among participants who were not sufficiently active to reach 100 PAI in the 80s, but who had increased to over 100 PAI by the mid-90s. In these participants, the reductions were 26% for dementia-related death and 17% for new-onset dementia, when compared to those who had less than 100 PAI at both measurement times.
In addition, we made separate analyzes for those who had high blood pressure, smoked or were overweight when they took part in the survey in the 1980s. In all these groups, we found that those who maintained their PAI score above 100 or increased from below to above 100 PAI during a ten-year period had a lower risk of developing dementia or dying from dementia during the follow-up period. Achieving 100 PAI was also more closely linked to dementia risk than meeting the health authorities' minimum recommendations for physical activity.
Older adults with poor cardiorespiratory fitness seem to be able to reduce the use of medication for anxiety, depression and sleep problems by improving their fitness. For those who already have a high maximum oxygen uptake, it seems less appropriate to further increase fitness.
The results are based on data on drug use and fitness among over 1,500 participants in the Generation 100 study. We measured the fitness of all the 70–77-year-old participants four times over five years, and obtained information on the use of medicines from the Norwegian Prescription Database throughout the entire period.
We found the highest use of medication for mental disorders among the least fit participants. Thereafter, the use of such drugs was gradually reduced with better fitness, up to a fitness number of 40 ml/kg/min. For the small number of participants who had even better cardiorespiratory fitness than this, drug use increased somewhat again.
The results were similar when we analyzed the use of antidepressants separately. On the other hand, we found no definite connection between cardiorespiratory fitness and the use of sleeping pills or anti-anxiety drugs, respectively.
The wiring network in the brain was not better preserved in the Generation 100 groups that were offered organized exercise, compared with the participants who were advised to exercise on their own. Nevertheless, the results suggest that high fitness and high-intensity training are beneficial for maintaining better structure in this network.
Good signaling in the brain depends on intact nerve fibers and a thick layer of myelin that insulates these fibers. Together, nerve fibers and myelin form the white matter of the brain. In this study, we used MRI to examine the structural organization of white matter in 105 of the 70-77 year old participants in the Generation 100 project. The measurements were made at start-up and after one, three and five years of exercise follow-up, respectively.
Myelin ensures that molecules move along the nerve fibers instead of diffusing away from the fibers. A high degree of myelination therefore indicates good conduction capacity of nerve signals in the brain. Our results show that elderly people with high exercise capacity - in all three groups - had both a greater degree of myelinated nerve fibers and of molecules that moved along the nerve fibers. However, this correlation was strongest at start-up and after one year, and decreased after that.
The study also found a link between higher self-reported exercise intensity and better structure of the white matter of the brain. Here, too, the association was only present at the beginning of the study period. The results may be an indication that high-intensity training and high fitness protect against damage to the wiring in the brain in the elderly. At the same time, it may seem that this effect diminishes as one approaches 80 years.
In general, the findings agree well with other results on exercise and brain health from the Generation 100 project (see here, here, here, here and here).
High-intensity training leads to increased HDL-mediated nitric oxide production in the blood vessel wall of patients with heart failure with preserved pump function. Nitric oxide is essential for the ability of the blood vessels to dilate, an ability that is severely impaired in this disease. HDL particles in the blood - often referred to as the good cholesterol - can stimulate increased production of nitric oxide by binding to a specific receptor in the blood vessel wall. It is this property of the HDL particles that is enhanced by regular 4x4 interval training in heart failure patients, whereas the total levels of HDL in the blood are unchanged.
The HDL particles also increased their antioxidant capacity following regular high-intensity exercise. In line with this, it turned out that the interval training reduced the levels of an important marker for oxidative stress in the blood of the participants. This can be important in terms of reducing the degree of inflammation in the blood vessel wall and the risk of new cardiovascular events.
In diastolic heart failure, the heart is large and stiff, and the heart chambers have low ability to fill with blood. In the study, which includes 34 of the participants from the international OptimEx trial we have led, the patients were randomly assigned to 4x4 interval training, training with moderate intensity or to a control group that did not receive exercise follow-up. Before, during and after the exercise period, we took blood samples, isolated HDL particles from these samples, and performed experiments to see if the exercise changed the HDL particles' ability to initiate nitric oxide production.
During the three months of organized training follow-up, this ability only improved in the participants in the 4x4 group. However, the improvements were lost nine months later, after a period in which participants were encouraged to exercise on their own, but trained significantly less than they did during the first three months.
In people with heart failure, physical capacity is lower if kidney function is also impaired. This combination is called cardiorenal syndrome, and patients with this condition might also have less effect of endurance training than heart failure patients with normal kidney function.
Among 61 people with heart failure who participated in our study, 40 had reduced kidney function. These had on average a maximum oxygen uptake which was 3.5 ml/kg/min lower than the 21 who had normal kidney function. In addition, they walked almost 100 meters shorter on a 6-minute walking test. Even after adjusting for other factors that were different in the two groups, the difference in fitness and walking capacity was statistically significant.
All participants in the study first attended a two-day course called "Living with heart failure", where they among other things received advice on physical activity and exercise. Thereafter, half of the participants were randomly selected to be followed up with digital exercise sessions two days each week for the next three months. The exercise included high-intensity intervals, and each session lasted one hour.
After the three months, the participants with cardiorenal syndrome who did not receive exercise follow-up had reduced their maximum oxygen uptake compared to when the study started. Further, the cardiorenal patients in the exercise group did not improve their fitness. On the other hand, we saw a significant improvement in fitness among the participants with normal kidney function in the exercise group.
Both among people with type 2 diabetes and healthy people, we saw immediate impairments in heart function right after a session of 4x4 interval training. The impairments were mostly equal in both groups, suggesting that intensive exercise does not stress the heart more in people with diabetes. We know that regular exercise strengthens the heart, and usually the impairments that occur in the acute phase are transient, but we did not specifically examine that in this study.
The relatively small pilot study includes seven people with diabetes and seven otherwise similar people who did not have diabetes. They performed a 4x4-minute high-intensity interval session, directly followed by an exhausting test of maximum oxygen uptake. The hearts of all participants were examined with ultrasound just before the training session and 30 minutes after the session. The only thing that changed differently in the two groups was the thickness of the septum between the left and right ventricles at the point where the heart was maximally filled with blood. This wall increased in thickness in healthy people after the training session, which may indicate more fluid accumulation than in those who had diabetes.
We also took blood samples to see if the intensive exercise affected the blood sugar and the levels of troponin T – a marker of heart damage – differently in diabetes. However, there was nothing to indicate such a difference. Furthermore, the participants wore equipment that measured ECG for a whole day before and after the training session. Those with diabetes had far more arrhythmias in the form of extra heart beats than the healthy participants. This applied both before and after the training session, and an acute bout of exercise did not affect the number of extra beats the following day in any of the groups.
Increased fitness is linked to reduction of dangerous plaques for heart patients

Both heart patients who performed high-intensity intervals twice weekly, and patients who did not receive exercise follow-up, had more stable, less high-fat plaques in the heart's blood vessels after six months. The participants who increased their maximum oxygen uptake during the period achieved a more favorable plaque composition than those who had not increased their fitness. However, organized interval training was in itself no more effective than standard follow-up.
We used near-infrared spectroscopy to obtain very advanced images from inside the coronary arteries of the patients, and examined how the lipid content of the plaques changed over time. A high fat content in the core of the plaques makes them more vulnerable, and plaques that rupture can lead to heart attacks. The findings may indicate that increased fitness by exercise reduces the amount of this dangerous fat in the blood vessels of the heart.
All 60 participants in the study had recently been treated for coronary artery disease. Half were randomly drawn to join the exercise group, which attended supervised interval training with the 4x4 method two days a week for six months. The control group received regular exercise advice without an offer of direct follow-up. As more than half of the participants in the control group improved their cardiorespiratory fitness during the period, we suspect that a good number of them nevertheless increased the amount of exercise after joining the study.
Although we did not find any difference in plaque content in the two groups after six months, both groups had less high-fat plaques than at baseline. Moreover, both groups had increased the levels of the good HDL cholesterol. The interval training also led to increased fitness compared to the control group, as well as reduced body weight and waist circumference.
We have uncovered two new genetic variants that appear to be important for the VO2 max level in women. Based on our own fitness measurements of over 4,500 Norwegians, we found 38 genetic variants that were linked to high or low maximum oxygen uptake. When we looked at the same variants in blood samples from 60,000 fitness-tested Britons, we could confirm that two of them were decisive for the fitness level - at least in women.
The analysis is a so-called genome-wide association study, where we have examined the entire genetic material of participants in the HUNT3 Fitness study. Thus, we have been able to analyze 14 million genetic variants in these participants to see if they are linked to their fitness level. In the population as a whole, only two of these variants were significantly associated with fitness. However, when we analyzed women and men separately, we found 35 potential fitness genes in women and two in men.
Two of the gene variants that were important for VO2 max in Norwegian women were also significantly related to fitness in the British population. One of the genetic variant is located in a gene that is important for heart function and development of cardiovascular disease. Poor fitness is closely linked to an increased risk of lifestyle diseases, and part of the explanation can probably be found in our genes.
Most studies that have looked for fitness genes in the past have either not measured fitness with a maximum test on a treadmill with direct O2 measurements, or had few participants. Thus, this is the first large study that can use a sufficiently strict level of statistical certainty to uncover genes that are most likely directly linked to fitness. In addition, the study has revealed a number of candidate genes, which may have an impact on fitness but must be investigated further in other studies.
The Generation 100 study showed no effect of organized exercise follow-up on avoiding age-related changes in the structure of different parts of the brain. On the other hand, the participants who started the study with high aerobic capacity had better preserved structural complexity of cerebral gray matter - and specifically in the temporal lobe - compared with those who were less fit.
Better maintenance of fitness throughout the five years of the study was also associated with better preserved structure in the temporal lobe. This area of the brain is sensitive to physiological aging and the development of Alzheimer's disease.
In Generation 100, three groups of older women and men exercised differently, with two of the groups being offered organized exercise twice weekly. This substudy includes the 105 participants who underwent MRI scans of the brain before and during the study. A new method was used to assess structural complexity more accurately in different parts of the brain.
After five years, the measurements of structural complexity showed equal reductions in all three exercise groups. But a high maximum oxygen uptake was linked to better preserved complexity in parts of the cerebrum. The level of fitness had, however, no effect on the thickness of the cerebral cortex.
The results are largely reminiscent of other recently published findings on exercise and brain health based on the Generation 100 study. The general conclusion seems to be that high age-related fitness can be a key to maintaining important brain functions and avoiding wasting of brain tissue for the elderly.
The higher fitness level you get with our popular Fitness Calculator, the lower is the risk of having to undergo surgery to open narrow blood vessels in the heart. And when fitness is good, the probability of a long life is higher for those who have had heart surgery.
The study is based on over 45,000 Norwegians who participated in the second wave of the Nord-Trøndelag Health Study in the mid-1990s. None of them had previous heart disease. We calculated the fitness of everyone with the formula from the Fitness Calculator.
By the end of 2017, 672 of the participants had went through heart surgery due to a heart attack or angina. The risk was 11% reduced for each increase of 3.5 fitness numbers, which is also called 1 MET. In addition, people who reported being very physically active had a 26% lower risk than the least active.
466 of the 672 who had heart surgery survived the entire follow-up period. The probabillty of survival was 15% higher for each 1 MET increase in fitness level. Among those who had heart surgery, the fifth with the highest fitness levels in the 1990s had less than half the risk of premature death, compared with those with the lowest fitness.
We have found four micro-RNA molecules that change levels after a period of exercise, and which are also associated with reduced plaque burden in the coronary arteries of heart patients. The results come from a study in which 31 patients either trained intensive intervals or with moderate intensity three days a week after they had opened narrow blood vessels in the heart. We examined their vessels with intravascular ultrasound both before and after the exercise period.
Micro-RNAs are tiny particles that regulate the activity of our genes. Many micro-RNA molecules are involved in various stages of the atherosclerosis process that clog blood vessels and lead to cardiovascular disease. In this study, we pre-defined 13 micro-RNA molecules that we examined further, based on results from previous studies.
After three months of training, the levels of micro-RNA-146a-5p had increased, while the levels of micro-RNA-15a-5p, 93-5p and 451a had decreased. All of these changes were also linked to a reduction in the total amount of plaque in the blood vessels of the patients. The study can not say anything about causation, but we can speculate that exercise leads to changes in micro-RNA that are beneficial in reducing coronary artery plaques in heart patients.
In addition, we found that the levels of six micro-RNA molecules were linked to a larger necrotic core. This plaque core consists of inflammatory cells and fat, and plaques with a lot of fat are more vulnerable to rupture that leads to heart attacks. However, changes in this necrotic core after an exercise period were not related to how micro-RNA levels changed during the same period.
The pumping function of the heart's right ventricle is somewhat reduced in people who have been hospitalized with severe covid-19 disease a few months ago, compared to otherwise similar people from the general population. The right ventricle pumps blood out into the pulmonary circulation, and the function was worst among the patients who had been admitted to the intensive care unit. More of the corona patients also had impaired filling of blood between each heart beat.
The study, which is led by our researcher Charlotte Björk Ingul in collaboration with researchers from five Norwegian hospitals, includes a total of 204 people who were admitted with covid-19 between February and June 2020. Each participant was matched with one person who was examined with cardiac ultrasound as part of the Nord-Trøndelag Health Study. Thus, the two groups were similar in terms of age, gender, BMI, blood pressure, previous heart and lung diseases, and diabetes. The corona patients also wore equipment that measured ECGs for 24 hours. 27% of them had cardiac arrhythmias three months after admission, mainly premature ventricular contractions and non-sustained ventricular tachycardia. No one developed atrial fibrillation after their covid-19 disease.
The lipoprotein profile of healthy people with low maximum oxygen uptake is similar to the lipoprotein profile of people with insulin resistance. We know that persons with low cardiorespiratory fitness have an increased risk of cardiovascular disease, and an unfavorable lipoprotein profile appears to be a probable part of the explanation. The results are based on data from the fitness testing of 211 healthy, middle-aged Norwegians who participated in the HUNT3 Fitness project. Half had high fitness, while the other half had low fitness, despite the fact that both groups were the same age and reported the same level of physical activity.
In the study, we used advanced nuclear MRI technology to study the levels of fats in 99 subgroups of the lipoproteins HDL, LDL, VLDL and IDL. Especially in the largest of the VLDL particles, we found increased levels of lipids such as cholesterol and triglycerides in those with low fitness. This group also had 15% higher VLDL levels overall. In addition, they had higher fat content in small LDL and HDL particles. HDL particles are often referred to as "good cholesterol" because they can protect against atherosclerosis, but this probably only applies to large and medium-sized HDL particles. Small LDL particles can also play an important role in the formation of harmful plaques in blood vessels.
We found no beneficial effect of high fitness or long-term organized exercise on the development of white spots in the brain of older adults. These spots can be seen on MRI, and are common after the age of 50. The spots are scars in the wiring in the brain, and are associated with impaired gait function, cognitive impairment, depression and stroke. Neither in the participants who were offered organized interval training with high intensity, nor in those who could attend moderate training sessions, did the growth of these scars develop differently than in those who exercised on their own.
The study includes 105 of the participants in the Generation 100 study. Their brains were checked with MRI before, during and after the five-year exercise period. The extent of white spots increased in all three groups, especially during the last couple of years of the 5-year period. The other three studies we have published on brain health in the Generation 100 study show that high fitness protects against cognitive impairments. However, we found no association between fitness and the development of white spots. Nor did those who improved their fitness during the study have slower development of white spots in the brain than the rest of the participants.
Blood plasma from exercised mice gives older, untrained mice better brain health. Recently, we initiated the ExPlas study, where we investigate whether people who have already developed Alzheimer's disease can benefit from plasma from fit, young donors. In a new review article, we address all previous research on exercise, fitness and Alzheimer's disease, and also look at the mechanisms that may explain why exercise that increases fitness can be an effective medicine to prevent and treat dementia.
We know a lot of molecules that are secreted directly in the brain when we exercise, or that are secreted into muscles or other tissues and transported to the brain with the blood. Several of them can break through the blood-brain barrier and contribute to better brain health. Treatment that increases the levels of these molecules can potentially revolutionize the treatment of Alzheimer's disease. Several of these molecules seem to affect each other, and there is likely much more complex interplay between them than what is known today. It is therefore not to be assumed that just one of these molecules could be used to mimic the beneficial effects of exercise training on brain health. We have more faith in a systemic approach with injection of blood plasma from well-trained donors, to better mimic real exercise and bring all its beneficial effects for the brain.
Physical inactivity contributes to one in four dementia cases in Europe. People with high levels of physical activity – especially those who have been active all their lives, exercise regularly with high intensity and are in good shape – have a significantly reduced risk of cognitive impairment and Alzheimer's disease. Exercise and high fitness can also delay the development of disease in people in the early stages of Alzheimer's disease.
Part of the exercise effect on the brain is probably due to the fact that exercise also affects the cardiovascular system beneficially. Among other things, it will increase blood flow to the brain and stimulate the formation of new brain cells and new blood vessels. In animal studies, exercise also reduces the levels of proteins that are essential in the development of Alzheimer's disease, including β-amyloid and hyperphosphorylated tau. In addition, the anti-inflammatory effect of exercise, as well as exercise effects on the energy-producing mitochondria, can play an important role.
We have discovered a new gene transcript that helps counteract the loss of muscle mass as we get older by stimulating the growth of fast, explosive muscle fibers. The levels of the RNA strand CYTOR in skeletal muscle increase after strength training, but decrease as we age. However, by using very advanced gene editing technology, we were able to increase the production of CYTOR and stimulate muscle-building processes in precursors of muscle cells from older people. In mice with muscle wasting due to manipulated low Cytor levels, gene editing led to increased Cytor levels, and muscle mass and strength was restored. And when we cloned human CYTOR into the roundworm Caenorhabditis elegans, we delayed the aging process so that the worms retained stronger, more functional muscles, moved faster and lived longer than worms that did not receive the same treatment. Thus, we may have laid the foundation for a new form of treatment to counteract muscle loss in the elderly.
The vast majority of our genetic material does not encode protein sequences, and CYTOR is a long, non-coding RNA strand found in this so called dark DNA of skeletal muscle cells. Among the many non-coding RNA transcripts that altered expression in the thigh muscles of humans after strength training, we found that CYTOR levels changed the most. We then showed that exercise increases the levels of Cytor in skeletal muscle in mice and rats, and that high Cytor levels help to preserve strong, explosive type II muscle fibers. We also found that older people with a specific gene variant that increases the levels of CYTOR have higher walking capacity than those who have other variants of this gene. The study is a collaborative project between CERG and two research groups in Switzerland and Denmark.
The exercise follow-up in the Generation 100 study may have given older men, but not older women, better cognitive function and a lower probability of mild cognitive impairment. Both men and women who maintained or increased their fitness during the study had better brain health than those with lower fitness levels, regardless of whether they were part of the groups that had received organized training follow-up or not. The greater the increase in fitness, the lower the likelihood of having mild cognitive impairment.
The study includes 945 of the 70-77 year old women and men who participated in the Generation 100 study. They had been randomly assigned to five years of exercise follow-up with intensive or moderate intensity, respectively, or to self-training. After the training period, they completed the MoCA test, which, among other things, tests short-term memory, executive function and ability to orientate in time and space. The men who had been part of the training groups scored higher on the test than the men in the control group, and they also had a 32% lower probability of mild cognitive impairment. Participants whose cardiorespiratory fitness decreased during the study had a 35% higher probability of mild cognitive impairment than those who maintained or improved their fitness over the five years.
Chinese men and women with a physical activity level of 100 PAI or higher have a 13–16% lower risk of dying from cardiovascular disease, compared to Chinese who are less active. The risk of death by all causes is also 7% lower, and with 100 PAI or more one could expect to earn almost three years of life. The relationship between PAI and risk of death can apparently not be explained by other differences between active and inactive people, as the analyzes have been adjusted for a number of such differences. The results show that PAI is a useful activity target also in a non-Western population.
The study uses data from a biobank with health information from almost 450,000 healthy men and women from ten different regions of China. Between 2004 and 2008, they reported their exercise habits and had a number of other health variables measured, such as blood pressure, BMI and blood sugar. 22,000 of the participants died over the next eight years, including 9,500 as a result of cardiovascular disease. 100 PAI was also linked to lower risk of premature death among smokers, people with high blood pressure, people with diabetes and the obese.
The organized exercise follow-up in the Generation 100 study did not make the participants better at solving cognitive tasks. Neither the group that was offered moderate intensity exercise sessions nor those who attended intensive interval training regularly for five years performed better than the control group. For example, all groups' abilities to remember the location of an object and memorizing words were similar. Moreover, the exercise follow-up had no effect on planning, the ability to separate similar memories or process information quickly. It is worth noting that the 70-77 year old participants on average had the same cognitive abilities after five years as at the start of the study, and they even improved on some of the tests.
In addition, we saw that the participants with high cardiorespiratory fitness at the start of the study, had better cognitive abilities throughout the study than those with lower fitness. We also saw an improvement in the so-called working memory, which concerns remembering and processing information while performing cognitive tasks, among the participants who improved their fitness during the study period. The study includes 106 of the Generation 100 participants, and they conducted cognitive tests on a web-based portal both at start-up and after one, three and five years.
Five years of organized exercise follow-up for older women and men in the Generation 100 study, did not reduce risk factors for cardiovascular disease significantly, compared to exercising on your own. After three years, however, a score for overall cardiovascular risk was significantly lower in the group that performed intervals with high intensity, and we saw a tendency for the same also after five years. Organized interval training for five years also resulted in better cardiorespiratory fitness, lower resting heart rate and lower BMI.
The main results from Generation 100 showed higher survival than expected among the 70-77 year old women and men who participated, and especially in the group that was randomized to interval training. The 1567 participants in the study were randomly divided into three groups, who were either offered to attend interval training or moderate training two days each week, or received general advice on moderate physical activity. The new research article examines whether traditional risk factors such as waist circumference, blood pressure, cholesterol profile and blood sugar changed differently in the three groups, and interval training tends to be most effective in improving the overall levels of these risk factors. Those who were offered moderate exercise sessions had no greater effect than those who were advised to be active on their own. A good number of participants in all groups trained differently than they were asked during the period, which makes it challenging to interpret the results. At the start of the Generation 100 study, the levels of risk factors were also healthier than we usually see in the elderly, which may also be an explanation for why we did not find major changes or differences between the groups.
High-intensity interval training could increase HDL cholesterol in older men

The men in the Generation 100 Study who performed 4x4 intervals with high intensity twice weekly increased their levels of HDL cholesterol by more than 6 % during the first three years of the study. After five years, the levels were still almost as high as when the study started. In comparison, HDL levels decreased by 6-7 % in the men who exercised at moderate intensity or were adviced to follow the general exercise recommendations. The HDL particles removes cholesterol from the blood vessel walls, and higher levels could reduce the risk of cardiovascular diseases.
In women, HDL cholesterol levels decreased by 2.6% after five years of interval training, compared to around 7% in the other two groups. However, the difference between the groups was not statistically significant. On the other hand, the men and women who improved their cardiorespiratory fitness the most, also had the most beneficial change in HDL cholesterol levels during the study. The Generation study recruited 1567 older adults aged between 70 and 77, and this particular analysis includes the approximately 50% who actually exercised according to the study protocol.
Levels of micro-RNA-181c were increased in heart failure patients whose fitness did not improve substantially after three months of exercise. Furthermore, the lower initial levels of micro-RNA-181c, the higher was the increase in maximal oxygen uptake during the intervention. The study includes patients with diastolic heart failure, meaning that the hearts fill so poorly with blood that they are unable to pump enough blood to the rest of the body. The findings may indicate that heart failure patients with high levels of micro-RNA-181c need other types of rehabilitation to increase fitness.
The study includes 51 participants from Antwerp and Munich who were drawn to one of the exericse groups in our large multi-center OptimEx study. The included patients all completed at least 70% of the exercise sessions. For 30 of them, the exercise did not lead to any major increase in the maximum oxygen uptake, while the last 21 were defined as exerice responders with an increase in fitness of at least 6.4%. First, we examined the levels of 377 different micro-RNAs in seven responders and seven non-responders of the same age and gender, and found higher levels of ten of the mico-RNAs in the non-responders. When we examined the same ten micro-RNAs in the rest of the participants, only micro-RNA-181c was elevated.
Almost a third of severely ill covid-19 patients had less than 80% of their age-expected fitness level three months after being discharged from hospital. For two-thirds of those who measured low fitness, there was no other obvious reason than decontioning following the disease - which emphasizes the importance of exercise and rehabilitation after covid-19. A minority had limitations in lung function, and some others had problems with heart ischemia or arrhythmias at maximum exertion. The study does not answer whether these are late effects of covid-19, or whether these participants also had the same limitations before the pandemic.
The study, which is a collaboration between five Norwegian hospitals, includes cardiopulmonary fitness tests of 156 covid patients without COPD or cardiovascular disease. Just over a third were women, and the average age was 56 years. 20% had been admitted to the intensive care unit, and this group had a somewhat lower maximum oxygen uptake than the rest. Almost half reported that they were still short of breath after three months, but these did not have worse lung function than the rest. On the other hand, they had a higher BMI and a lower maximum oxygen uptake per kilogram of body weight than those who reported no dyspnea.
Organized exercise follow-up did not prevent loss of brain cells compared to giving general exercise advice without offering organized exercise sessions. However, Generation 100 participants with high cardiorespiratory fitness at the onset of the study had thicker cerebral cortex throughout the five-year exercise period than those who were less fit.
To check for changes in brain volume and the thickness of the cerebral cortex, we performed MRI scans of the brains of 105 of the 70-77 year old participants in the Generation 100 study both before, during and after the exercise intervention. The group that exercised on their own without organized follow-up had less than age-expected atrophy of the hippocampus and the foremost part of the brainstem. In the groups exercising at high and moderate-intensity, respectively, the atrophy was somewhat greater than among those who exercised on their own, but still not higher than what is expected for people in their 70s.
Distance walked on a six-minute walking test gives - together with age, gender and score on a functional independence test - a fairly good estimate of future cardiorespiratory fitness for people who have recently suffered a stroke. About 60% of the variation in maximum oxygen uptake 18 months after the stroke is explained by these four factors, compared to approximately 50% if the model does not include the gait test. Adding maximum walking speed to the model, however, does not improve it further.
90 largely independent stroke patients participated in the study. Three months after the stroke, they performed the walking tests and wore an accelerometer for four days. Then they took part in an exercise study before they came back to test their fitness18 months later. The results also show that the most physically active walked longer on the test, had a higher maximum walking speed, and measured a higher maximum oxygen uptake one and a half years later. However, these relationships were so weak that they are unlikely to have clinical significance. Our researcher Inger-Lise Aamot Aksetøy has contributed to the study, which was mainly carried out by the NTNU research group GeMS.
We're more prone to infections the first days after a really hard workout. Intensive exercise leads to acutely increased production and excretion of inflammatory markers, also in the heart's left atrium. It is also known that some of these markers affect the structure of the atrium and the electrical signals in the heart in a way that can trigger arrhythmias. At the same time, more moderate amounts of exercise can chronically strengthen the immune system and reduce the vulnerability to infections.
This is a field where there is still a lack of knowledge, but in this new article we summarize what is currently known about how the immune system responds to exercise and may affect the risk of developing atrial fibrillation. More research in this area could possibly help to uncover mechanisms for why hard exercise over many years probably increases the risk of getting atrial fibrillation, while regular training in more normal amounts lowers the risk.
24 treadmill sessions of high-intensity interval training enabled stroke patients to walk 40 meters longer in six minutes than before the training period. They also improved their balance compared to the group that received standard care without exercise training. The 4x4 interval training also increased the ability to complete the Trail-Making Test - which requires the ability to recognize letters and numbers, good eye coordination and general motor skills - and this effect was also present after a full year. At 12 months follow-up, however, it was surprisingly the participants in the control group who reported being most functionally independent.
The results are from the same study that last year showed that 4x4 intervals improve fitness after stroke. Exercise did not affect health-related quality of life, global cognitive function or symptoms of anxiety and depression. A total of 56 relatively young and healthy patients who had had a stroke during the last five years before the training period completed the study.
Eating a carbohydrate-rich meal before a 5-6 minute running test can extend the time to exhaustion by about half a minute, compared to performing the test fasting or after eating less sugars. This applies both to very well-trained men and to men with below average cardiorespiratory fitness. However, the intake of carbohydrates before the test does not affect the maximum oxygen uptake, the threshold for when lactic acid starts to accumulate in the blood, or the work economy. Thus, the study does not answer which physiological mechanisms cause high carbohydrate intake to improve running performance.
The study includes 21 men, eleven of whom were endurance athletes who trained at least once every day. The participants performed three identical endurance tests on three different days - in random order. Before the highest-performing test, they ate a meal consisting of white bread, jam, oatmeal, banana and raisins equivalent to 3 grams of carbohydrates per kilogram of body weight. The other two tests were performed on an empty stomach and after a meal consisting of yogurt, almonds and avocado, respectively. This meal contained as many calories as the carbohydrate-rich meal, but the content of sugars was only 0.5 grams per kilogram of body weight.
People with COPD have higher cardiorespiratory fitness if their lung function is less impaired. The less air the participants managed to exhale in one second, the lower the maximum oxygen uptake. This applied to both patients with and without emphysema, but the association between lung function and fitness appears somewhat greater in emphysema. The group of patients with the highest degree of emphysema also had the worst lung function and the lowest VO2max.
The results suggest that mechanisms that impair lung function in patients with COPD also contribute to lower cardiorespiratory fitness. The study includes data from 186 patients with COPD who were tested at a specialist clinic in Telemark, Norway between 1999 and 2014. In contrast to previous studies in the field, our study has taken into account that lung volume varies based on gender, age and height.
In collaboration with researchers from a number of other countries, we uncovered 12 genes that can potentially determine whether one responds well or poorly to endurance training. However, when we tried to confirm these gene variants using data from other studies, we found no definite correlations. Thus, we need better studies with far more participants before we can possibly predict exercise response based on genes, and it is possible that our genes play less of a role than we have thought.
The research collects data on exercise response from 18 different studies with a total of 507 participants. Many genes showed tendencies to be related to training response, but only 12 showed such a strong link that they were examined further in a new group of 39 participants. In this group, however, none of these 12 gene variants were closely linked to exercise response. We also examined 97 gene variants that have previously been linked to endurance training response. A few of these also showed positive, but far from certain, associations in our data material.
Several mechanisms that regulate protein degradation in skeletal muscle are disrupted in patients with heart failure. This probably contributes to the muscle loss that is common in these patients. The study compares two groups of patients with heart failure; one with reduced pump function, and another with intact pump function but large and stiff hearts that fill poorly with blood between beats.
The research uses data from 40 German patients who participated in the large international SMARTEX-HF and OptimEx studies, both of which were led by CERG. Blood samples and muscle biopsies from patients have also been compared with 12 healthy but untrained individuals. The muscles of both groups of failure patients had increased activity of substances that degrade proteins and leads to loss of muscle mass. The activity was highest in the half of the patients with the lowest cardiorespiratory fitness. The participants with reduced cardiac pump function had lower fitness than expected for their age, which can possibly be linked to the fact that mitochondrial function was most impaired in this group.
Mice lacking the enzyme heme oxygenase-1 in skeletal muscle do not respond to endurance training. Such enzyme deficiency also leads to loss of muscle mass and to mitochondrial dysfunction. During exercise, micro-ruptures cause heme to be released in muscle cells and blood. High levels of heme are toxic, and heme oxygenase-1 breaks down heme inside muscle cells.
The study, which was conducted by Harvard researchers, uses data from experiments our leader Ulrik Wisløff has conducted with rats born with either high or low physical capacity. The results show that the fit rats have lower levels of heme and higher levels of heme oxygenase-1 in the skeletal muscles than the rats with low fitness. The researchers further show that endurance training causes the levels of heme oxygenase-1 to increase. This mechanism likely protects the muscle cells from injury, and helps the cells to respond to endurance training.
Physical capacity, lung function and right ventricular function are improved by eight weeks of high-intensity interval training immediately after treatment for pulmonary embolism. Our leader Ulrik Wisløff is last author of a pilot study conducted in Iran, and the results suggest that patients with pulmonary embolism can benefit from participating in rehabilitation groups with a focus on high-intensity training. The study is the first to look at the effect of such training for this group of patients, who often suffer from shortness of breath and low physical capacity for a long time.
Half of the 24 patients were randomly selected to participate in the group that attended 24 interval training sessions after they had been discharged from the hospital. The participants completed a total of eight two-minute intervals per sessions, with a heart rate of 80-90% of maximum. After eight weeks, they had reduced their resting heart rate by 14% and increased the physical capacity by 65% on an exhausting treadmill test. They were also able to exhale more air in one second than the participants in the control group, and had improved the function of the right ventricle, which pumps blood to the lungs. The training also improved the health-related quality of life of the patients.
High cardiorespiratory fitness is associated with high blood volume, high hemoglobin mass and a high volume of red blood cells in the elderly. The link between blood volume and fitness can be partly explained by the fact that older people with good fitness are more physically active than less fit elderly people. The amount of physical activity did however not affect the relationship between fitness, red blood cells and hemoglobin mass. This agrees well with what we already know that physical activity can increase blood volume, whereas genetic predisposition probably has the greatest significance for hemoglobin mass and red blood cell volume.
It is well known that high blood volume is crucial for high maximum oxygen uptake and good endurance performance among athletes, but this study is among the first to show that this relationship also applies to healthy elderly people. 50 participants from the Generation 100 project participated, half of whom were in good shape for their age, while the rest had a low maximum oxygen uptake. We measured their blood volume using so-called CO re-breathing, where you inhale a certain amount of carbon monoxide mixed with pure oxygen for two minutes. We also took blood samples from the participants and equipped them with an activity monitor for seven days to find out how physically active they were.
Both intensive interval training three days a week and moderate-intensity training five days a week reduced calcium leakage in heart muscle cells in rats with diastolic heart failure. However, the moderate exercise also led to several other improvements in calcium handling, as well as significantly improved stroke volume and filling of blood between each heartbeat. Good calcium handling is important both for the contractility of the cells and for limiting the risk of dangerous arrhythmias.
Patients with diastolic heart failure have large and stiff hearts that fill poorly with blood. Our new results show that rats with diastolic heart failure have somewhat impaired calcium handling compared to healthy rats. Two-thirds of the rats with heart failure then trained either 4x4-minute intervals or moderate-intensity training for eight weeks, before the groups were compared with each other and with the non-exercising control group. 12 rats completed this exercise part of the study.
Levels of cardiac troponin T were reduced after both 12 weeks and one year of exercise in chronic heart failure patients. Troponin T leaks from damaged heart cells, and the levels in the blood are used to diagnose both chronic and acute cardiac damage. Our new results are based on 213 participants in the large international SMARTEX-HF exercise trial. The improvements took place in the groups that exercised under supervision, as well as in the control group that were adviced to be active on their own. We also found a clear association between higher cardiorespiratory fitness and lower troponin T levels, suggesting that exercise that improves fitness is important for limiting heart damage in patients with chronic heart failure.
Some have been concerned that high-intensity exercise could exacerbate the damage to the heart in people with chronic heart failure, but our results show that this is not the case. One group in SMARTEX-HF trained 4x4-minute high-intensity intervals under supervision for three months, while the other training group exercised with steady, moderate intensity. The groups then continued to exercise on their own for the next year.
Healthy women and men who are physically active enough to achieve at least 100 PAI every week for decades gain less weight than people who are inactive. Overweight and obesity contribute to nearly five million deaths each year worldwide, and our study suggests that the PAI activity metric may help attenuate unhealthy weight gain.
The results are based on data from more than 85,000 healthy persons who participated in at least one of the three waves of the Nord-Trøndelag Health Study (HUNT) arranged between 1984 and 2008. On average, body weight increased by approximately 8 kilos in the men and women who participated in both HUNT1 and HUNT3. Weight gain was significantly lower among those who were physically active enough to obtain at least 100 weekly PAI on all three occations. Also participants who were inactive in the 1980s, but had increased the amount of activity to at least 100 PAIs in both the 1990s and 2000s, gained less weight than their inactive counterparts.
The fitness calculator we have developed specifically for patients with rheumatoid arthritis gives a good indication of life expectancy in this patient group: Lower fitness means higher risk of premature death. Three quarters of all people with rheumatoid arthritis have lower estimated cardiorespiratory fitness than average for their gender and age. The low average fitness levels largely explains why these patients generally live shorter than most people.
The study contains data from 348 persons with and 60,938 people without arthritis. All participated in the second or third wave of the Nord-Trøndelag Health Study in the 1990s and 2000s. More than a third of the participants with arthritis died by the end of 2018, compared to just a fifth of the other participants. After taking into account differences in age and the most common risk factors, the risk of premature death was still increased by 28% for arthritis patients. 5% of the increased risk could be attributed to the rheumatic disease, while as much as 23% was related to the low fitness level in the group with rheumatoid arthritis.
For patients with heart failure with preserved ejection fraction, three months of 4x4 high-intensity interval training three days a week gave the same increase in maximal oxygen uptake as moderate exercise of longer duration five days a week. However, it is unclear whether the improvements are large enough to be clinically important for the patients. A total of 180 patients participated in the OptimEx study, where we collaborated with five other European universities.
Both the participants who trained intervals and moderately improved their cardiorespiratory fitness 1-2 ml/kg/min more than the participants who did not take part in organized exercise. However, after another nine months of home-based training the improvements were no longer statistically significant in any of the exercise groups. The exercise had no effect on cardiac function or structure, whereas participants in all three groups reported that their quality of life improved during the year of the study.
Comparable effects of high-intensity interval training in women and men with heart disease

High-intensity interval training improves relative cardiorespiratory fitness similarly in women and men with coronary heart disease, according to a new meta-analyses. Six of 16 included studies are from our research group, and our researcher Inger-Lise Aamot Aksetøy has contributed to the paper. Female patients are greatly underrepresented in studies of high-intensity interval training after a heart attack, and sex-specific analysis could not prove a significant effect on cardiorespiratory fitness compared to moderate intensity exercise.
Cardiorespiratory fitness in absolute terms improved more in male than female patients. Furthermore, the meta-analysis shows that high-intensity interval training might impact blood sugar and body weight less in women than men with coronary artery disease. However, the effects are not different across sexes when it comes to blood pressure or lipid profile.
A study of healthy Americans confirms what we have previously shown among Norwegians: Those who exercise enough to maintain a PAI score of 100 or more have a lower risk of premature death and death due to cardiovascular disease, and they can expect to live almost five years longer than those who do not exercise. Even inactive people who over time increase their activity level to at least 100 PAI can expect better health. PAI is a standard for physical activity level developed by us at CERG.
The study includes nearly 18,000 men and women who participated in repeated health surveys in Dallas, Texas between 1974 and 2002. We calculated their PAI scores from the first and last survey based on their self-reported activity levels. After the last survey, they were followed for a median of almost ten years. Those with 100 PAI or more at both surveys had 51% reduced risk of dying from cardiovascular disease and 42% reduced risk of all-cause deaths compared to those who were physically inactive. Those who increased the amount of activity from 0 to at least 100 PAI between the two measurements had 25% and 18% reduced risk of cardiovascular death and overall death, respectively.
Estimated cardiorespiratory fitness decreases faster in people with rheumatoid arthritis than in the general population. Using the fitness calculator we have developed specifically for this patient group, we calculated fitness for 188 rheumatoid arthritis patients who participated in both the second and third wave of the Nord-Trøndelag Health Survey. We did the same with the original Fitness Calculator in more than 26,000 men and women without rheumatoid arthritis. During the eleven years between the health surveys, estimated cardiorespiratory fitness decreased by 8.3 ml/kg/min for the participants with rheumatoid arthritis, compared to 6.7 for people of the same age from the general population.
A total of 436 persons with rheumatoid arthritis participated in at least one of the two health surveys. These had 2–5 ml/kg/min lower estimated fitness to begin with than equally old participants from the rest of the population. The decrease in fitness for those who participated in both surveys was highest in the older age groups, and this effect was even greater among those with rheumatoid arthritis. Smoking, cardiovascular disease, higher BMI, asthma and hypertension were also associated with a faster decline in fitness.
Only 3% of participants in the high-intensity interval training group died during the five-year exercise period of the Generation 100 Study. In the group that exercised with moderate intensity, approximately 6% died. The expected mortality for Norwegians in this age group is 10%. Thus, the results indicate that older adults live longer if they are able to maintain a high physical activity level, and that high-intensity exercise could be extra effective. Interval training also improved fitness and quality of life to a greater extent than moderate training.
The high-intensity training in the study consisted of two weekly sessions of 4x4 intervals, and nearly 400 of the 70-77-year-old participants were randomized to this group. Another 400 were randomized to exercise moderately for two days a week. Both groups were offered group sessions twice weekly but could also choose to perform most of the exercise sessions by themselves. In addition, both groups were advised to be physically active with moderate intensity for 30 minutes most other days of the week. The study also includes a control group who received regular exercise advice and were followed up with regular health and fitness tests. This group actually reported to exercise more with high intensity than the moderate group but less than the high-intensity group. Approximately 4.5% of the participants in the control group died during the five-year period.
Men and women who preserve their maximum oxygen uptake well over a ten-year period also have a healthier development of risk factors for cardiovascular disease than those who have a greater decline in cardiorespiratory fitness. Moreover, regular exercise with high intensity is linked to better maintained fitness. The results signal that high-intensity training is effective in slowing down age-related loss of fitness and reducing the risk of lifestyle diseases.
Between 2006 and 2008, we conducted gold standard maximum oxygen uptake test of more than 4,000 healthy Norwegians. Ten years later, we tested approximately 1,500 of the same people again. On average, cardiorespiratory fitness was reduced by 10% in women and 12% in men, and the decrease was greatest in the highest age groups. In inactive persons, the fitness decreased by 15% on average, whereas participants who reported exercising with moderate intensity for at least 150 minutes a week had a decrease of 9%. Among those who exercised for at least 75 minutes at high intensity every week, the oxygen uptake decreased by only 5%. Furthermore, those who maintained their fitness best had less adverse changes in cholesterol profile, blood pressure, resting heart rate and waist circumference.
Exercise makes the heart healthier in many ways in rats with heart failure following a major heart attack. High-intensity interval training is more effective than moderate training. After 6–8 weeks of near-daily sessions with intensive four-minute intervals, the rats with failure in our study actually achieved higher cardiorespiratory fitness than healthy, sedentary rats. The heart's ejection fraction, which was initially severely impaired, also increased considerably, and several measures of heart stiffness and pathological thickening of the heart muscle approached normal levels as a result of the high-intensity training. The group of rats that exercised with moderate intensity did as much total work as the interval training group and also had several beneficial effects of training, but these were generally less pronounced than in the high intensity group.
Heart failure leads to susceptibility of severe heart arrhythmias, but the study suggests that interval training in particular can reduce this risk significantly. We only managed to induce ventricular fibrillation in one of 14 rat hearts that had not had a heart attack, while all the untrained hearts with heart failure got ventricular fibrillation. In the interval training group, arrhythmia was only triggered in one of nine failing hearts, compared with five of eight hearts in rats that had trained moderately. The study, which we conducted in collaboration with the Group of Molecular and Cellular Cardiology, also reveals several of the mechanisms behind the exercise effects, including normalization of micro-RNA levels, improved calcium handling inside heart muscle cells, and improvements in the heart's electrical system.
Older adults in Norway are slimmer than older adults in Brazil, and also have better grip strength and less triglycerides in the blood. Most seniors in both countries report being physically active at least two days each week. Norwegian older adults in general have higher cholesterol levels and blood pressure than Brazilians, but the proportion who use blood pressure medication is more than twice as high among Brazil's elderly. According to the study, an equally high proportion in both countries have the metabolic syndrome, which is an accumulation of risk factors for cardiovascular disease.
The differences in BMI and waist circumference seem to be explained by the fact that older people in Norway have a higher level of education than older people in Brazil. There was no difference when we repeated the analyzes without including the Brazilians who had no secondary education. 310 participants from our Generation 100 study and 255 seniors from Ribeirao Preto in Brazil are included in the study. 80% are women.
The main reason why endurance training improves maximum oxygen uptake is that it enables the heart to pump more blood with each beat. Stroke volume increases in part because exercise makes the heart muscle bigger, thicker and stronger, so that the heart empties better for each stroke. In addition, exercise improves the heart's ability to fill with blood between each beat, partly because its chambers become more elastic. Exercise can even reverse some of the impairments and damages we see in the function and structure of diseased hearts, for example after a heart attack. Exercise also increases activation of the parasympathetic nervous system, and this contributes to both lower resting heart rate and improved heart rate variability.
In a new article published in Nature Metabolism, our researchers summarize the physiological effects of exercise on the heart, as well as some of the molecular mechanisms that explain the beneficial adaptations. Research on these mechanisms is very important for development of effective cardiac drugs for people who are unable to exercise physically. Much research is still to be done in this field, but we know that endurance training leads to reprogramming of thousands of genes that are important for the heart. A trained heart has increased capacity to burn fatty acids, and several of the underlying mechanisms have been mapped all the way down to the molecular level. The same is true regarding exercise effects on several molecules that make the heart bigger and stronger.
Healthy Americans who reach 100 weekly PAI or more can expect to live four years longer than their physically inactive peers. Our new, popular activity standard PAI (Personal Activity Intelligence) has previously been linked to a longer and healthier life among participants in the Nord-Trøndelag Health Study, but this is the first time we have examined this in a population from another country.
The new study includes comprehensive health data and self-reported activity information from over 56,000 women and men who participated in the renowned Aerobics Center Longitudinal Study in Dallas, Texas between 1974 and 2003. More than 3,000 of them died during the study period, and the risk was reduced by about 20% for women and men with an activity level of 100 PAI or more. The risk of dying from cardiovascular disease was even more profoundly reduced. The association between 100 PAI and a longer life was valid for people of all ages, and also for smokers and people with high blood pressure, high blood sugar, obesity or adverse cholesterol levels.
4x4 high-intensity interval training for 12 weeks appears to improve diastolic heart function during exercise for people who have recently had a heart attack. Diastolic heart function tells how well the heart fills with blood between two beats. The improvement occurred despite the fact that the study participants had fairly well preserved cardiac function. We did not see any change in the pumping or filling function of the heart at rest after the exercise period.
Participants inproved fitness substantially during the training period, and improved their maximum oxygen uptake by almost 4 mL/kg/min on average. We also showed that maximum oxygen uptake was closely linked to diastolic heart function during exercise. The study includes 28 patients who either trained on their own or met at the hospital for group-based circuit or treadmill training two days each week.
Endurance training counteracts muscle wasting and prolongs life in rats with cancer. Compared to healthy animals, tumor-bearing rats had lung edema, high levels of oxidative stress and severe cancer-related loss of muscle mass (cachexia). Exercise did not affect the size of the tumor, but normalized lung edema, improved several markers of oxidative stress, increased running performance and slowed death. Importantly, endurance exercise also attenuated muscle mass atrophy and fully restored muscle contractile function to the same level as cancer-free animals.
Most of the experiments were conducted on rats performing daily 3x4-minute aerobic interval training. However, continuous moderate training improved running capacity and lifespan just as much as interval training in rats with cancer. Thus, it is likely that the other observed benefits of exercise in tumor-bearing rats also apply to moderate intensity exercise. Our researchers Jose Bianco Moreira and Ulrik Wisløff have contributed to the research article.
Maximum oxygen uptake increases with increased lung function in patients with heart attack or angina, even among patients with healthy lungs. We included 93 patients with established coronary artery disease and lung function within the normal range. The more air the participants were able to breathe out during one second after filling their lungs completely, the higher fitness they had. We also measured the diffusion capacity of oxygen from alveoli to blood, and this measure of lung function was also associated with cardiorespiratory fitness.
Our lungs play an important role for transport of oxygen from the air to our blood vessels. However, they are not considered an important limiting factor for maximum oxygen uptake in persons with healthy lungs. In our study, none of the patients had low oxygen saturation in their arteries at the end of the exhausting exercise test, and most did not reach their maximal breathing capacity. Thus, ventilatory or gas exchange limitations do probably not explain the link between lung function and fitness. Neither do age, sex, body mass index, smoking nor medication. We hypothesize that an interplay between the respiratory and circulatory systems affects the maximal capacity to transport oxygen from air to muscle during maximum exercise, but more research is needed to reveal relevant mechanisms.
A single high-intensity interval training session provides immediate improvement in blood vessel function and blood pressure in adolescents, and the effect is greater than after a moderate training session. Blood sugar control and insulin sensitivity also improve acutely after intensive interval training, which also reduces the accumulation of fats in the blood after a meal. However, these effects are not greater than with moderate intensity exercise. Adolescents can experience interval training more fun than moderate exercise.
Our researcher Charlotte Björk Ingul is one of the experts in The British Association of Sport and Exercise Sciences, which has now issued a research-based statement summarizing what we know about intensive interval training for children and adolescents. They emphasize that more research is still needed on the chronic effects of this form of exercise among young people. For obese children and adolescents, there are indications that interval training is more effective than less intensive exercise in terms of improving fitness, while blood pressure, waist measurements, insulin resistance and cholesterol profile seem to improve equally with both forms of exercise. It is unclear whether high-intensity interval training can contribute to weight loss in overweight children and adolescents.
Only two published studies to date have looked at how high-intensity interval training impacts human brain circulation. This obviously needs to be studied more extensively, but based on its superior effect on cardiorespiratory fitness, we believe that interval training could be even better for brain health than moderate exercise.
CERG's professor Ulrik Wisløff has joined a group of international researchers to sum up the current knowledge on high-intensity interval training and brain health in a scientific review. The suggestion is that greater improvements in cardiorespiratory fitness could simply confer additional neuroprotection through a translational dose-response effect, and promote healthy ageing by delaying stroke, cognitive decline and dementia with corresponding benefits for individuals, their families and society in general.
Interval training reduced plaques most effectively in stented vessels
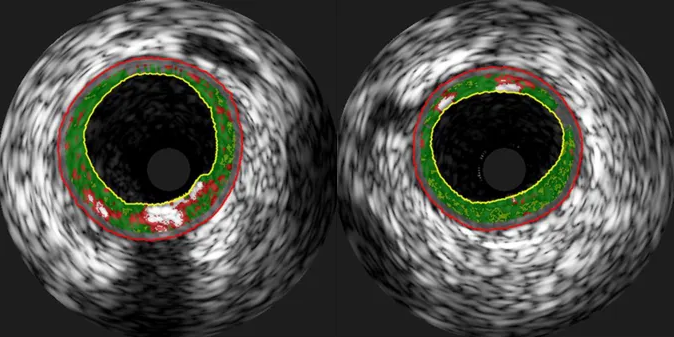
4x4 interval training after treatment for heart attack or angina can have a greater effect on plaque burden in the stented coronary arteries than moderate intensity exercise. Also, the content of the vulnerable necrotic core in the middle of the plaques was reduced more with interval training in our study. This core of dead tissue is a marker for risk of plaque rupture and a new heart attack. In a previously published article from the same study, we showed that exercise seems to reduce plaques also in the non-stented part of the coronary arteries. However, those analyses found no difference between interval training and moderate exercise.
Thirty-two patients with stable coronary artery disease participated in the study, and were randomly assigned to the two exercise groups. All participants were treated with modern drug-eluting stent implantation before the exercise intervention. We used intravascular ultrasound to examine the stent itself, as well as the 0.5 cm areas outside of both edges of the stent. Only plaques outside the distal stent edge showed favourable changes after the 12-week exercise period. Both exercise groups achieved significant reductions in plaque burden and necrotic core in this area, but the effects were greatest for the high-intensity interval training group.
Eight weeks of organized high-intensity interval training improves cardiorespiratory fitness in stroke survivors. However, the long-term effects on fitness and health are more uncertain.
The randomized controlled HIIT-Stroke study was performed at three specialized rehabilitation centres in Norway, and followed up 56 patients one year after half of them had completed 24 training sessions of 4x4 intervals. The 8-week exercise period improved maximum oxygen uptake significantly but one year later the VO2max had decreased towards baseline values again. It was, however, still higher compared to the control group, although the difference only reached statistical significance for relative (mL/kg/min) and not absolute (L/min) VO2max. The exercise did not affect blood pressure, blood lipids or insulin sensitivity, which may not be surprising since participants had healthy values even before the study started.
Regular physical activity and high cardiorespiratory fitness seem to protect against premature death and cardiovascular events in people with atrial fibrillation. Both exercise at moderate and high intensities are associated with substantially reduced risk. When compared with inactive men and women without atrial fibrillation, we found increased health risk among inactive atrial fibrillation patients, but not among active patients. Today, there are no specific exercise guidelines for people with atrial fibrillation, but our study clearly indicates that this group should also exercise regularly to limit the risk of cardiovascular events and early death.
We included 1117 patients who had atrial fibrillation when they participated in the third HUNT Study between 2006 and 2008. Their average age was just above 70 years, and we followed them until November 2015. Those who reported exercising in line with official recommendations had almost half the risk of dying compared to those who exercised less. The results were similar for deaths from cardiovascular disease. We used the Fitness Calculator to estimate the fitness of the participants, and found that the risk of dying during follow-up decreased by 12 % for each increase of 1 MET (3.5 fitness numbers). For cardiovascular deaths, this risk reduction was 15 %.
We have found six new genetic variants that link closely to having high or low cardiorespiratory fitness. Having a higher number of the favourable genetic variants – and a lower number of the bad ones – is linked to lower waist circumference, fat percentage, BMI and blood lipid levels. Furthermore, to have good fitness genes is associated with a lower likelihood of using blood pressure medication. We know that genes are quite important for maximum oxygen uptake, and this is the first major study to look for genetic variants associated with directly measured cardiorespiratory fitness.
In the study, we analyzed more than 120,000 unique genetic variants in 3470 healthy women and men who measured their maximum oxygen uptake during the HUNT3 Fitness study. We found that 41 of the genetic variants were closely related to the fitness of these participants, even after adjusting for gender, age and self-reported activity level. Six of the same genetic variants were also significantly associated with high fitness in the validation cohort of 718 elderly who participated in the Generation 100 study. Further experiments indicated that the genetic variants in question affect gene expression in adipose tissue, skeletal muscle and heart.
The left atrium is larger in healthy adults with good cardiorespiratory fitness, compared to healthy adults with poorer fitness. A large left atrium is one of the criteria for diastolic dysfunction – where the heart's ability to fill with blood between beats is reduced – but our study shows no association between atrial size and diastolic heart function. The results indicate that fitness should be taken into consideration when assessing if left atrial volume is a sign of future heart disease: In persons with low cardiorespiratory fitness, increased atrial volume is probably a bad sign. In fitter persons, it's not necessarily so.
The result are based on data from 242 healthy women and men who participated in the HUNT3 Fitness Study, and who also had their hearts examined with cardiac ultrasound as part of the HUNT3 Study. The association between fitness and atrial size was especially strong in the oldest age groups. We also studied if self-reported physical activity is linked to atrial size, but this association was weaker than what we found for fitness level.
Our Fitness Calculator is not as accurate for men and women with rheumatoid arthritis as for most people. Now, we have contributed to a new fitness formula based on maximum oxygen uptake tests of 93 persons with rheumatoid arthritis. This new formula estimates fitness far better in this group of patients than the original Fitness Calculator – especially in those with low fitness. We recommend health professionals to use the new calculator to assess fitness in persons with rheumatoid arthritis and to motivate these patients to become more physically active.
Try the new Fitness Calculator for rheumatoid arthritis
To use the calculator, you need information on disease activity over the past week. However, we have also made an alternative formula that can be used in case you don't have that information. This formula is available in the abstract of the research paper.
Average fitness in males aged between 20 and 29 years is 49 mL/kg/min. Fitness decreases by approximately 9 % every decade. In all age groups, women have around 25 % lower cardiorespiratory fitness than men. The results are based on almost 12,000 directly measured treadmill tests of maximum oxygen uptake. More than 3500 of these tests are from the HUNT3 Fitness Study, whereas the rest are from the US and Canada. The goal is to establish global age-specific refererence values for cardiorespiratory fitness in men and women.
The results also show that Norwegian men and women have significantly higher fitness levels than people from Northern America. The article also includes previously published fitness data from Brazil, Israel and Japan, and neither of these countries have equally high cardiorespiratory fitness levels as Norway.
A medium fit 20–29-year-old male heart pumps 21 milliliters of oxygen with every beat at maximum exertion. From that, the peak O2 pulse decreases every decade, and at 80–89 years of age the blood pumped with each beat only contains 11 milliliters of oxygen. We also see the same downward trend in women: The maximum O2 pulse among medium fit women in their 20s is 14 milliliters, whereas it is only 8 milliliters among medium fit women in their 80s.
In collaboration with a group of American researchers, we present reference values for maximum O2 pulse in healthy men and women of all ages. The results are based on more than 13,000 treadmill tests of maximum oxygen uptake, of which more than 4000 were conducted during the HUNT3 Fitness Study. Maximum O2 pulse is a marker of the stroke volume of the heart and says a lot about the heart's pumping capacity during exercise. Exercise tests can be used for health assessment, and the results from this study makes it easy to compare the results from individual tests with normative values.
Younger patients with less severe heart failure are more likely to respond to three months of endurance exercise than older and sicker patients. In the SMARTEX Heart Failure trial, the odds of improving cardiorespiratory fitness was seven times worse for patients in NYHA class III, where symptoms are present even at slight physical activity, compared to patients in NYHA class II. Cardiac function at baseline also mattered, and the lower pumping capacity of the heart, the less was the chance of responding to the exercise program.
An important prerequisite for improving fitness during the training period was that exercise load was gradually increased over the three months. SMARTEX-HF is a large international exercise trial coordinated by us. Although the main results published in 2017 indicate small overall effects following both interval training and continuous exercise, the new article shows that significantly more participants improved their fitness in the two exercise groups than in the control group.
Both those who maintain high cardiorespiratory fitness and those who improve their fitness over time have about half the risk of incident dementia, compared to those with consistently low fitness. Moreover, the risk of dying of or with dementia is substantially reduced if your fitness is high. We have followed more than 30,000 Norwegians for up to 30 years, and men and women who scored high on the Fitness Calculator in both the 1980s and 1990s had 44% lower risk of dementia-related death by June 2016. Those who were among the 20% with the poorest fitness in 1980s but no longer belonged to this group in the 1990s, had nearly 30% reduced risk. A total of 814 people died of or with dementia during the period.
The Health and Memory Study in Nord-Trøndelag confirmed that 310 of the HUNT participants developed dementia between 1995 and 2010. For each 1 MET increase in fitness between the two HUNT surveys, the risk of incident dementia was 16% lower. Further analyzes showed that you can expect 2–3 extra years of life without dementia if you improve your fitness.
Six weeks of exercise led to increased ATP levels in cardiomyocytes of rats with heart failure, but the ratio between phospocreatine and ATP did not change. ATP releases energy for muscular work, and phosphocreatine is necessary to rebuild ATP – and the phosphocreatine/ATP ratio expresses the levels of high-energy phosphates within heart muscle cells. Failing hearts have lower levels of high-energy phosphates, giving less potential to generate energy and decreased pumping capacity. Neither moderate exercise nor high-intensity interval training influenced the phosphocreatine/ATP ratio in our study.
However, the exercise increased the maximum oxygen uptake, cardiac performance and mitochondrial respiraton, which shows that the exercise actually was effective in improving cardiac metabolism. Thus, the study indicates that the phosphocreatine/ATP ratio is not suited to evaluate the beneficial effects of exercise in the heart. A total of 30 rats were included in the study, of which half had heart failure following a myocardial infarction and were randomized to high-intensity, moderate or no exercise.
By measuring the levels of five different micro-RNA molecules, we could improve risk prediction of myocardial infarction in healthy persons. The 10-year risk of a heart attack could be calculated with the Framingham model, which includes several common risk factors for cardiovascular disease. However, our study indicates that this model could be substantially improved by adding measurements of micro-RNA 21-5p, 26a-5p, 29c-3p, 144-3p and 151a-5p. Micro-RNAs are miniscule molecules that regulate the activity of most genes in our body.
The study includes 96 men and women who had a heart attack within ten years, despite being healthy when they attended the Nord Trøndelag Health Study in 1995–97 (HUNT2). The levels of ten different micro-RNAs were compared to the levels of 99 age- and gender-matchen persons who stayed healthy during the ten years following HUNT2.
Men and women with high estimated fitness have reduced risk of atrial fibrillation. Furthermore, those who improve their fitness over time have 44 % lower risk than those with declining fitness levels. The results are based on data from almost 40,000 participants in the third HUNT Study, and their fitness was estimated with our Fitness Calculator. The findings suggest that high fitness and exercise to improve fitness reduce the risk of atrial fibrillation.
During eight years of follow-up, more than 1000 of the participants had a confirmed diagnosis of atrial fibrillation. The fifth of women with highest estimated fitness for their age only had half the risk compared to those with lowest fitness. In men, the risk was reduced the most among those in the second highest quintile of fitness. We looked at change in fitness among 22,000 participants who also had taken part in the HUNT2 Study eleven years earlier, and found a close link between increased fitness and lower risk of atrial fibrillation.
To be physically active over time seems to protect against adverse health concequences of gaining weight. Compared to weight stable persons who were regularly physically active for at least 10 years, those who increased their body weight by more than 5 % had no increased risk of early death if they were physically active during the same time period. On the other hand, those who gained weight and were physically inactive over time had more than 50 % increased risk, whereas weight stable inactive persons had a lower risk increase.
The study uses data from the first two waves of the Nord Trøndelag Health Study. In total, 34,000 women and men were asked about the activity habits both in the mid-1980s and 1990s. The participants were followed until the end of 2013, and by then almost 8500 had died. More than 3000 died from cardivascular causes, and also cardiovascular mortality was increased only in physically inactive persons who gained weight.
Those with rheumatoid arthritis who have low cardiorespiratory fitness also have higher body mass index, are less physically active, more often smoke and have higher blood pressure and resting heart rate than patients with higher fitness levels. Moreover, both men and women with rheumatoid arthritis generally have lower fitness than healthy persons of the same age. A low level of physical activity and overweight are the factors that seem to contribute the most to lower cardiorespiratory fitness, and the results highlight that exercise to increase fitness is important to improve cardiovascular health in persons with rheumatoid arthritis.
Higher disease activity was not linked to lower cardiorespiratory fitness in our study. Further, only 10 % of the participants reported that the fitness test to exhaustion resulted in arthritis-related leg pain. These findings might indicate that other factors than the disease per se influence the motivation for physical activity in this group of patients. In the study, we have measured maximum oxygen uptake in 93 men and women with rheumatoid arthritis and compared the results with healthy participants from the HUNT3 Fitness Study.
High cardiorespiratory fitness could be even more protective against a first myocardial infarction in women than in men. The third of middle-aged and older women with the highest fitness estimated with our Fitness Calculator had 25 % reduced risk of myocardial infarction during the next 13 years compared with the women with the lowest fitness, even after accounting for other differences between the groups. The 10 % risk reduction we found in fit men was not statistically significant.
We used data from 26,163 healthy women and men aged above 50. They participated in the second wave of the Nord-Trøndelag Health Study, HUNT2 in the mid-1990s. By the end of 2010, 1566 of the participants had their first myocardial infarction. The risk was 3 % and 11 % lower for every increase of 3.5 mL/kg/min in men and women, respectively.
A large increase in creatine kinase is a normal phenomenon after intensive exercise, and three of 24 young, healthy participants in our study got a confirmed diagnosis of rhabdomyolysis. Rhabdomyolisis is characherized by muscular pain, leakage of creatine kinase from muscle cells to blood, and myoglobin in urine. The condition involves muscle swelling and potential kidney damage, and is regulalry treated with intravenous fluids. Our study indicates that well-hydrated healthy persons with exercise-induced rhabdomyolysis are less likely to develop kidney damage, and might not need the same treatment as those who get rhabdomyolsis from other causes.
All the young students in our study had a marked increase in creatine kinase in blood four days after a very intense exercise session of Tabata intervals. Three fulfilled all the criteria for rhabdomyolysis. The increase in creatine kinase was highest in those with the lowest frequency of strength training prior to the experiment.
Men who exercise regularly have as high mitochondrial respiration in their thigh muscles as world-class cross-country skiers. The mitochondria are the main source of energy production in the musculature, and the results indicate that the mitochondrial function is only trainable up to a certain level. They also indicate that the capacity of the heart is the main factor accounting for the higher aerobic capacity in elite skiers during whole-body activities.
On the other hand, the 13 cross-country skiers in the study had much higher mitochondrial respiration in their upper arm musculature compared to the twelve regular exercisers in the control group. We also showed a strong correlation between upper arm mitochondrial respiration and peak oxygen uptake during arm cycling. These results show that the ability to utilize oxygen in the musculature is crucial for the aerobic capacity during upper-body activites, which activates so little muscle mass that the heart has no problem supplying enough oxygen. They also indicate that regular runners have a huge potential to increase their upper body mitochondrial respiration.
The higher levels of C-reactive protein (CRP) in blood, the poorer cardiorespiratory fitness. CRP levels indicate general inflammation, and high CRP is considered a risk factor for cardiovascular disease. The results might indicate that poor fitness contributes to increased inflammation, and that exercise to improve aerobic capacity could affect CRP levels positively.
We used data from more than 1400 women and men that had their cardiorespiratory fitness tested during the third wave of the Nord-Trøndelag Health Study (HUNT3). About half of them had the metabolic syndrome, characterized by central obesity and at least two more risk factors for cardiovascular disease. Higher CRP was also associated with metabolic syndrome and increased body mass index.
Eight weeks of high-intensity interval training ameliorated some, but not all, mitochondrial dysfunctions in the hearts of mice with type 2 diabetes. Mitochondrial respiration is the main source of energy production in our muscles, but individuals with diabetes have smaller and less effective mitochondria. The exercise protocol in our study fixed several of the impairments in mitochondrial respiration. Furthermore, after the exercise period, the mitochondria of mice with diabetes were no longer significantly smaller than in healthy mice.
During cellular respiration, electrons are transported through four protein complexes in the so-called electron transport chain in the mitochondria. The activity in complexes I, II and IV was attenuated by up to 50% in the diabetic mice, but exercise corrected the impairments in complexes II and IV. The exercise, however, did not repair the mitochondria's reduced ability to absorb calcium, which is also important for effective cellular respiration. The study included 17 healthy mice and 30 mice genetically predisposed to developing diabetes. Half of the mice with diabetes trained 10x4-minute intervals at 90% of maximum capacity five days a week for eight weeks.
Improved cardiorespiratory fitness is linked to higher brain volumes. 751 men and women aged between 50 and 67 years had their brains scanned as part of the HUNT3 study between 2006 and 2008. The same persons also participated in the HUNT2 study eleven years earlier, and those who maintained high fitness or improved from low to high between the two surveys had bigger brains than those who stayed unfit.
We estimated fitness with our Fitness Calculator. High fitness seems to be good for brain volume also for persons with symptoms of anxiety or depression. The results support exercise aimed to improve cardiorespiratory fitness as an important public health initiative to maintain brain health among middle-aged individuals.
Heart failure is associated with several impairments in cardiac and skeletal muscle metabolism. The changes are linked to reduced contractility, muscle wasting and ineffective, anaerobic energy production. Our results indicate that the metabolic changes that occur in the heart during heart failure is mainly caused by the disease, whereas exercise to a larger extent affects skeletal muscle metabolism.
We have used advanced nuclear magnetic resonance imaging in six groups of rats, of which half had surgically established heart failure. The healthy and sick rats were randomized to one sedentary and two exercise groups of different intensity. Our analyses found several changes in the metabolism of cardiomyocytes in failing rat hearts, and very few of these changes were affected by exercise. On the other hand, mainly exercise training – and not heart failure – altered the metabolite distribution in skeletal muscle.
Exercise reprograms genes in the failing heart towards a healthier profile. We found 932 genes that were significantly affected by heart failure in rats that did not exercise. In exercised rats, only 174 genes differed in abundance compared to the healthy control group. Moreover, we identified nearly 50 genes that were differently expressed in exercised compared to not exercised failing rat hearts.
We chose 16 genes for further analysis. Many of them proved to be affected by heart failure also in humans, and we especially identified the enzyme proline dehydrogenase as an interesting target for future gene therapy. The expression of this enzyme is reduced in heart failure, but increases with exercise. When we silenced the gene in heart muscle cells from humans, the levels of the heart failure marker BNP doubled. On the other hand, when we stimulated to overexpression of proline dehydrogenase, processes that are important for energy production and metabolism increased significantly.
Several studies indicate that physical activity and high cardiorespiratory fitness can protect against Alzheimer's disease and dementia in general. In this review we sum up the evidence, and also highlight some potential mechanisms explaining why exercise and high fitness could be protective.
Exercise reduces cardiovascular risk factors, such as obesity, hypertension and diabetes, all of which are also risk factors for dementia. However, exercise and high fitness could potentially also reduce dementia risk directly, by promoting the formation of new blood vessels and neurons in the brain, as well as preserving brain volume. The review highlights nine factors that are released into the bloodstream in response to physical activity and support growth, survival, and differentiation of neurons and blood vessels.
Men and women with 100 weekly PAI or more have significantly higher cardiorespiratory fitness than those with less than 100 weekly PAI. Obtaining 100–150 weekly PAI seems to secure having the average cardiorespiratory fitness expected for your age and sex. PAI (Personal Activity Intelligence) is our new standard for activity tracking, and 100 weekly PAI is associated with better health and a longer life.
In this new article, we review the existing evidence on PAI, and supplement them with new analyzes linking gradually increasing PAI scores to higher cardiorespiratory fitness in more than 3,000 healthy men and women who performed a direct test of maximum oxygen uptake. The findings suggest that PAI could be a useful tool to motivate people to become sufficiently physically active to improve their health.
We found that the 20 % with the lowest cardiorespiratory fitness had 17 times higher likelihood of having non-alcoholic fatty liver disease compared to the 40 % with the highest fitness, even among individuals who sat less than four hours a day. Furthermore, among the 36 % who had non-alcoholic fatty liver disease in our cohort, the risk of dying within the next nine years was 50 % higher in those with low fitness.
Our results also show that cardiorespiratory fitness is much stronger linked to non-alcoholic fatty liver disease than sedentary time and adhering to official physical activity recommendations. The study includes 16,000 men and women who participated in the Nord-Trøndelag Health Study (HUNT) between 2006 and 2008.
Cross-country skiers should not do isolated upper-body work like double poling to improve their cardiorespiratory fitness. We have shown that the peak heart rate and O2 pulse during intensive seated double poling is too low to tax the cardiovascular system sufficiently. The peak oxygen uptake during double poling was far lower than during running and diagonal skiing, whereas the blood lactic acid concentration at a given heart rate was higher.
12 male elite cross-country skiers performed three sessions with different modes of exercise at gradually increasing intensities, followed by a test to exhaustion. The power output during high-intensity seated upper-body double poling was not high enough to have a likely effect on fitness. The results indicate that it's not the heart that limits exercise performance during maximal upper-body work, but rather local muscular fatigue.
High-volume high-intensity interval training is more likely to improve cardiorespiratory fitness than continuous exercise at moderate intensity. One third of those who performed regular interval training with at least 15 minutes of high intensity per session increased their fitness, even when we used strict criteria to define a likely response. In comparison, one fifth of those who exercised at moderate intensity for at least 30 minutes per session were responders.
The article includes data from 18 trials and 677 participants from five countries. We have included studies with healthy adults of all ages, as well as higher risk populations and patients with coronary heart disease. A gain of at least 5 ml/kg/min was defined as response to exercise. The studies with the longest duration and highest exercise loads had the most significant number of responders, indicating that at least some of those who were deemed non-responders would respond with an increase in training duration, frequency or intensity.
Lung function could be important for the physical capacity even in healthy adults. We studied the association between forced expiratory lung volume in one second (FEV1) and maximum oxygen uptake in 741 individuals aged 20 to 79 years, and found a linear relationship between better lung function and higher fitness in men, women, young, elderly and non-smokers.
Everyone included in the study had a lung function within the normal limits. Dynamic lung volume is not considered a limiting factor of oxygen uptake in healthy persons, and most of our participants had preserved ventilatory reserve at the end of their peak fitness test. Even so, our results suggest that lung function affects maximum oxygen uptake, and the potential mechanisms need to be studied further in the future.
List of scientific publications
2026:
Eriksen, E. A., Nauman, J., Wisløff, U., Omland, T., & Stensvold, D. (2026). Cardiorespiratory fitness and physical activity and risk of SARS-CoV-2 and COVID-19 hospitalization: the HUNT study. BMC Infectious Diseases.
2025:
Øvretveit, K., Klevjer, M., Brumpton, B. M., Wisløff, U., Hveem, K., & Bye, A. (2025). Polygenic prediction of cardiorespiratory fitness in the Trøndelag health study (HUNT). Scientific Reports.
Nauman, J., Ingeström, E. M., Tari, A. R., & Wisløff, U. (2025). Running from Death: Can Fitness Outpace Alcohol’s Harm? Changes in Alcohol Intake, Fitness and All-Cause Mortality in the HUNT Study, Norway Sports Medicine, 1-11.
Bakken, J., Brissach, D. E., Ingeström, E. M. L., Midttun, S., Walker, T. L., Stensvold, D., & Tari, A. R. (2025). Effects of 5-Year Exercise Training on Cognition in Older Adults: 10-Years Follow-Up from the Generation 100 Study. Sports Medicine - Open
Schellenberg, J., Matits, L., Kersten, J., Bizjak, D. A., Kirsten, J., Fremo, T., Tjønna, A. E., Skovereng, K., Sandbakk, Ø., & Letnes, J. M. (2025). Physiological assessment of left ventricular size indexed by peak oxygen uptake across sporting disciplines. European Heart Journal-Imaging Methods and Practice, qyaf138.
Vahle, B., Klädtke, R., Schauer, A., Bowen, T. S., Wisløff, U., Linke, A., & Adams, V. (2025). Skeletal Muscle Alterations in Different Phenotypes of Heart Failure with Preserved Ejection Fraction. International Journal of Molecular Sciences, 26(13), 6196.
Nordeidet, A. N., Marwarha, G. S., Røsand, Ø., Johansen, V., Garten, K., Høydal, M. A., Langaas, M., & Bye, A. (2025). Investigating the cardiorespiratory fitness gene COX7A2L in cardiomyocytes: Viability and mitochondrial function. PloS one, 20(6), e0326249.
Jacques, M., Landen, S., Sharples, A. P., Garnham, A., Schittenhelm, R., Steele, J., Heikkinen, A., Sillanpäa, E., Ollikainen, M., Broacth, J., Zarekookandeh, N., Hansson, O., Ekström, O., Asplund, O., Lamon, S., Alexanders, S. E., Smith, C., Bauer, C., Woessner, M. N., Levinger, I., Teschendorff, A. E., Gillberg, L., Blom, I., Helge, J. W., Harvey, N. R., Haupt, L. M., Griffiths, L. R., Deshmukh, A. S., Pietiläinen, K. H., Piirilä, P., Seaborne, R. A. E., Klevjer, M., Bye, A., Wisløff, U., Jones-Freeman, B., & Eynon, N. (2025). Molecular landscape of sex-and modality-specific exercise adaptation in human skeletal muscle through large-scale multi-omics integration. Cell Reports, 44(6).
Bekkos, C. H., Sujan, M. A. J., Stunes, A. K., Tari, A. R., Aagård, N., Brobakken, C. L., Brevig, M. S., Syversen, U., Wang, E., & Mosti, M. P. (2025). Acute effects of a single bout of high-intensity strength and endurance exercise on cognitive biomarkers in young adults and elderly men: a within-subjects crossover study. Journal of Translational Medicine, 23(1), 685.
Sagelv, E. H., Manskow, U. S., Antypas, K., Morseth, B., Aksetøy, I. L. A., Nes, B. M., Gagnon, M.-P., & Zanaboni, P. (2025). Online interventions to increase physical activity levels in self-reported inactive adults: the ONWARDS randomised controlled trial. BMJ Open Sport & Exercise Medicine, 11(2).
Amraei, Z., Ahmadizad, S., Fayaz Milani, R., & Wisloff, U. (2025). The effect of different exercise on the expression of cardiac anti-aging genes in myocardial tissue, sinoatrial node (SA) and atrioventricular node (AV) in elderly rats. Sport Physiology.
Solberg, E. E., Ingul, C. B., Edvardsen, T., Grimsmo, J., Haugaa, K. H., Loennechen, J. P., Nyrnes, S. A., Smedsrud, M. K., Vesterbekkmo, E. K., Ørn, S., & Mjølstad, O. C. (2025). Targeted cardiac screening of athletes. Tidsskrift for Den norske legeforening.
Parvan, R., Rolim, N., Gevaert, A. B., Cataliotti, A., van Craenenbroeck, E. M., Adams, V., Wisløff, U., Silva, G. J. J., & OptimEx Study Group. (2025). Multi‐microRNA diagnostic panel for heart failure with preserved ejection fraction in preclinical and clinical settings. ESC Heart Failure.
Solberg, A., Aspvik, N. P., Lydersen, S., Midttun, S., Reitlo, L. S., Steinshamn, S., Ingebrigtsen, J. E., Helbostad, J. L., Wisløff, U., & Stensvold, D. (2025). Effect of a 5-Year Exercise Intervention on Objectively Measured Physical Activity and Sedentary Time in Older Adults—The Generation 100 Study. Journal of Physical Activity and Health, 1(aop), 1-9.
Tari, A. R., Walker, T. L., Huuha, A. M., Sando, S. B., & Wisloff, U. (2025). Neuroprotective mechanisms of exercise and the importance of fitness for healthy brain ageing. The Lancet, 405(10484), 1093-1118.
Joensuu, L., Koivunen, K., Tynkkynen, N. P., Palviainen, T., Kaprio, J., Klevjer, M., Øvretveit, K., Wisløff, U., Bye, A., Ekelund, U., Sillanpää, E., & FinnGen Consortium. (2025). Genetic liability to sedentary behaviour and cardiovascular disease incidence in the FinnGen and HUNT cohorts. British Journal of Sports Medicine.
Dinges, S. M. T., Schwedhelm, E., Schoenfeld, J., Gevaert, A. B., Winzer, E. B., Haller, B., Baldassarri, F., Pressler, A., Duvinage, A., Böger, R., Linke, A., Adams, V., Pieske, B., Edelmann, F., Dalen, H., Hole, T., Larsen, A. I., Feiereisen, P., Karlsen, T., Prescott, E., Ellingsen, Ø., van Craenenbroeck, E. M., Halle, M., & Mueller, S. (2025). Effects of exercise training on nitric oxide metabolites in heart failure with reduced or preserved ejection fraction: a secondary analysis of the SMARTEX-HF and OptimEx-Clin trials. European Journal of Preventive Cardiology, zwaf142.
De Martin Topranin, V., Wiig-Fisketjøn, A., Botten, E., Dalen, H., Langaas, M., & Bye, A. (2025). Sex-specific cardiovascular disease risk prediction using statistical learning and explainable artificial intelligence: the HUNT Study. European Journal of Preventive Cardiology, zwaf135.
Müller, M., Hanssen, T. A., Johansen, D., Jakobsen, Ø., Pedersen, J. E., Aamot Aksetøy, I. L.,Rasmussen, T. B., Hartvigsen, G., Skogen, V., Henriksen, A., . & Thrane, G. (2025). Experiences with early aerobic interval training after heart valve surgery in patients with infective endocarditis. A qualitative study. European Journal of Physiotherapy, 1-8.
Gevaert, A. B., Winzer, E. B., Mueller, S., De Schutter, S., Beckers, P. J., Hommel, J., Linke, A., Wisløff, U., Adams, V., Pieske, B., Halle, M., van Craenenbroeck, E. M., & Van De Heyning, C. M. (2025). Training‐induced change of diastolic function in heart failure with preserved ejection fraction. ESC Heart Failure.
Hallan, S. I., Øvrehus, M. A., Shlipak, M. G., Potok, O. A., Romundstad, S., Aspvik, N. P., Wisløff, U., Ix, J. H., Stensvold, D., & Langlo, K. A. (2025). Long-Term Physical Exercise for Preventing CKD in Older Adults: A Randomized Controlled Trial. Journal of the American Society of Nephrology, 10-1681.
Wen, C. P., Chen, C. H., Nauman, J., Wai, J. P. M., Tsai, M. K., Lee, J. H., Chu, T-W. D., Ingestroem, E. M. L., Chiou, H. Y., Hsu, C. C. Wen, C., Wu, X, Tari, A. R., & Wisloff, U. (2025). Resting heart rate–The forgotten risk factor? Comparison of resting heart rate and hypertension as predictors of all-cause mortality in 692,217 adults in Asia and Europe. Progress in Cardiovascular Diseases.
Ingul, C. B., Hollekim-Strand, S. M., Sandbakk, M. M., Grønseth, T. I., Rånes, T. I. K., Dyrendahl, L. T., Eilertsen, K., Kristensen, S., Follestad, T., & Løfaldli, B. B. (2025). Empowerment in Type 2 diabetes: A patient-centred approach for lifestyle change. Diabetes Research and Clinical Practice, 220, 111998.
Nes, B. M., Letnes, J. M., Johnson, K. E., Sellevold, A. B., Byrkjeland, R., Brown, F. P., Follestad, T., Dalen, H., Wisløff, U., Løchen, M.-L., Tveit, A., Morseth, B., Myrstad, M., & Loennechen, J. P. (2025). Effects of 1-year exercise in patients with atrial fibrillation: study protocol for the Norwegian Exercise in Atrial Fibrillation (NEXAF) randomised controlled trial. Open Heart, 12(1).
Wai, J. P. M., Wen, C. P., Tsai, M. K., Chen, C. H., Lee, J. H., Chu, T. W. D., Chiou, H. Y., Wen, C., Tari, A. R., Wisløff, U., & Nauman, J. (2025). Association between activity quotient and cause-specific mortality–A prospective cohort study of 0.5 million participants in Asia. Progress in Cardiovascular Diseases.
2024:
Tari, A. R., Brissach, D. E., Ingeström, E. M., Nauman, J., Tyrell, T., Foster, C., Radtke. K., Porcari, J. P., Lydersen, S., Kaminsky, L. A., Myers, J., Walker, T. L., Coombes, J. S., Stensvold, D., & Wisløff, U. (2024). Survival of the fittest? Peak oxygen uptake and all-cause mortality among older adults in Norway. Progress in Cardiovascular Diseases.
Lundgren, K. M., Langlo, K. A. R., Salvesen, Ø., Aspvik, N. P., Mo, R., Ellingsen, Ø., Vesterbekkmo, E., Zanaboni, P., Dalen, H., & Aksetøy, I. L. A. (2025). Exercise-Based Telerehabilitation for Heart Failure Patients Declining Outpatient Rehabilitation-A Randomized Controlled Trial. Medicine and science in sports and exercise.
Nauman, J., Mirzaamin, T., Franklin, B. A., Nes, B. M., Lavie, C. J., Dunn, P., Arena, R., Weng, C. P., Tari, A. R. & Wisløff, U. (2024). Bolstering the Prognostic Utility of Coronary Risk Assessments with PAI: A Physical Activity Metric. Medicine and science in sports and exercise.
Svenningsen, A., Söderström, S., Bucher Sandbakk, S., Gullestad, L., Bønaa, K. H., Wisløff, U., & Hollekim-Strand, S. M. (2024). Mind the intention-behavior gap: a qualitative study of post-myocardial infarction patients’ beliefs and experiences with long-term supervised and self-monitored physical exercise. BMC Sports Science, Medicine and Rehabilitation, 16(1), 204.
Øvretveit, K., Ingeström, E. M., Spitieris, M., Tragante, V., Thomas, L. F., Steinsland, I., Brumpton, B. M., Gudbjartsson, D. F., Holm, H., Stefansson, K., Wisløff, U., & Hveem, K. (2024). Polygenic Interactions With Environmental Exposures in Blood Pressure Regulation: The HUNT Study. Journal of the American Heart Association, e034612.
Letnes, J. M., Nes, B. M., Sandbakk, Ø., Tjønna, A. E., Fremo, T., Moldjord, C., Høydal, M., Wisløff, U., & Dalen, H. Comparison of resting heart rate and left ventricular ejection fraction in elite endurance athletes and the general population. European journal of preventive cardiology, zwae294.
Geigenmüller, J. N., Tari, A. R., Wisloff, U., & Walker, T. L. (2024). The relationship between adult hippocampal neurogenesis and cognitive impairment in Alzheimer's disease. Alzheimer's & Dementia.
Dalen, H., Letnes, J. M., Hoydal, M. A., & Wisløff, U. (2024). Diastolic function and dysfunction in athletes. European Heart Journal-Cardiovascular Imaging, jeae155.
Bjørdalsbakke, N. L., Sturdy, J., Wisløff, U., & Hellevik, L. R. (2024). Examining temporal changes in model-optimized parameters using longitudinal hemodynamic measurements. BioMedical Engineering OnLine, 23(1), 64.
Berg, J., Nauman, J., & Wisløff, U. (2024). Normative values for body composition in 22,191 healthy Norwegian adults 20–99 years: The HUNT4 study. Progress in Cardiovascular Diseases, 85, 82-92.
Sabo, S., Dalen, H., Nyberg, J., Grenne, B. L., Jakobsen, E. O., Nes, B. M., Wisløff, U., & Letnes, J. M. (2024). Left atrial to ventricular volume ratio and relation to fitness, cardiovascular risk factors and diastolic function in healthy individuals. The HUNT Study. European Heart Journal-Imaging Methods and Practice, qyae028.
Lechner, K., Kia, S., von Korn, P., Dinges, S. M., Mueller, S., Tjønna, A. E., Wisløff, U., van Craenenbroeck, E. M., Pieske, B., Adams, V., Pressler, A., Landmesser, U., Halle, M., & Kränkel, N. (2024). Cardiometabolic and immune response to exercise training in patients with metabolic syndrome: retrospective analysis of two randomized clinical trials. Frontiers in Cardiovascular Medicine, 11, 1329633.
Kemi, O. J., Hoydal, M. A., Haram, P. M., Smith, G. L., Ellingsen, O., Koch, L. G., Britton, S. L., & Wisloff, U. (2024). Inherited physical capacity: Widening divergence from young to adult to old. Annals of the New York Academy of Sciences.
Nordeidet, A. N., Klevjer, M., Øvretveit, K., Madssen, E., Wisløff, U., Brumpton, B. M., & Bye, A. Sex-specific and polygenic effects underlying resting heart rate and associated risk of cardiovascular disease. European Journal of Preventive Cardiology.
Riveland, E., Valborgland, T., Ushakova, A., Skadberg, Ø., Karlsen, T., Hole, T., Støylen, A., Dalen, H., Videm, V., Koppen, E., Linke, A., Delagardelle, C., van Craenenbroeck, E. M., Beckers, P., Prescott, E., Hallen, M., Omland, T., Ellingsen, Ø., Larsen, A. I. &v SMARTEX‐HF Study Group. (2024). Exercise training and high‐sensitivity cardiac troponin‐I in patients with heart failure with reduced ejection fraction. ESC Heart Failure.
2023:
Klevjer, M., Rasheed, H., Romundstad, P. R., Madssen, E., Brumpton, B. M., & Bye, A. (2023). Insight into the relationship between resting heart rate and atrial fibrillation: A Mendelian Randomization study. Europace, 25(10), euad292.
Nystøyl, B. T. S., Letnes, J. M., Nes, B. M., Slagsvold, K. H., Wisløff, U., & Wahba, A. (2023). Cardiorespiratory fitness and the incidence of surgery for aortic valve stenosis–The HUNT study. European Journal of Cardio-Thoracic Surgery, ezad322
Letnes, J. M., Wisløff, U., & Dalen, H. (2023). Heart Failure With Preserved Ejection Fraction: Exercise Deficiency or Ventricular Maladaptation to Metabolic Demands?. Cardiovascular Imaging, 16(9), 1233-1235.
Tynkkynen, N. P., Törmäkangas, T., Palviainen, T., Hyvärinen, M., Klevjer, M., Joensuu, L., Kaprio, J., Bye, Anja & Sillanpää, E. (2023). Associations of polygenic inheritance of physical activity with aerobic fitness, cardiometabolic risk factors and diseases: the HUNT Study. European Journal of Epidemiology, 1-14.
Nordeidet, A. N., Klevjer, M., Wisløff, U., Langaas, M., & Bye, A. (2023) Exploring shared genetics between maximal oxygen uptake and disease: the HUNT study. Physiological Genomics
Norevik, C. S., Huuha, A. M., Røsbjørgen, R. N., Bergersen, L., Jacobsen, K., Miguel-dos-Santos, R., Ryan, L., Skender, B., Moreira, J. B. N., Kobro-Flatmoen, A., Witter, M. P., Scrimgeour, N., & Tari, A. R. (2023). Exercised blood plasma promotes hippocampal neurogenesis in the Alzheimer's disease rat brain. Journal of Sport and Health Science.
Williams, G. J., Al-Baraikan, A., Rademakers, F. E., Ciravegna, F., van de Vosse, F. N., Lawrie, A., Rothman, A., Ashley, E. A., Wilkins, M. R., Lawford, P. V., Omholt, S. W., Wisløff, U., Hose, R., Chico, T. J. A., Gunn, J. P., & Morris, P. D. (2023). Wearable technology and the cardiovascular system: the future of patient assessment. The Lancet Digital Health, 5(7), e467-e476.
Lundgren, K. M., Langlo, K. A. R., Salvesen, Ø., Zanaboni, P., Cittanti, E., Mo, R., Ellingsen, Ø., Dalen, H., & Aksetøy, I.-L. A. (2023) Feasibility of telerehabilitation for heart failure patients inaccessible for outpatient rehabilitation. ESC Heart Failure.
Johansen, K. R., Ranhoff, A. H., Sørensen, E., Nes, B. M., Bucher‐Sandbakk, S., Wilsgaard, T., Løchen, M.L., Morseth, B., & Myrstad, M. (2023). Ten‐year mortality among older male recreational endurance athletes in the Birkebeiner Aging Study in comparison with older men from the Tromsø Study. Scandinavian Journal of Medicine & Science in Sports.
Sæther, J. C., Vesterbekkmo, E. K., Taraldsen, M. D., Gigante, B., Follestad, T., Røsjø, H. R., Omland, T., Wiseth, R., Madssen, E., & Bye, A. (2023). Associations between circulating microRNAs and lipid-rich coronary plaques measured with near-infrared spectroscopy. Scientific Reports, 13(1), 7580.
Sperstad, S. B., Sæther, J. C., Klevjer, M., Giskeødegård, G. F., Bathen, T. F., Røsbjørgen, R., Dalen, H., & Bye, A. (2023). Lipoprotein subfraction profiling in the search of new risk markers for myocardial infarction: The HUNT study. Plos one, 18(5), e0285355.
Sæther, J. C., Vesterbekkmo, E. K., Gigante, B., Giskeødegård, G. F., Bathen, T. F., Follestad, T., Wiseth, R., Madssen, E., & Bye, A. (2023). The association between circulating lipoprotein subfractions and lipid content in coronary atheromatous plaques assessed by near-infrared spectroscopy. IJC Heart & Vasculature, 46, 101215.
Letnes, J. M., Nes, B. M., Langlo, K. A. R., Aksetøy, I. L. A., Lundgren, K. M., Skovereng, K., Sandbakk, Ø., Wisløff, U., & Dalen, H. (2023). Indexing cardiac volumes for peak oxygen uptake to improve differentiation of physiological and pathological remodeling: from elite athletes to heart failure patients. European Heart Journal-Cardiovascular Imaging, jead034.
Apelland, T., Janssens, K., Loennechen, J. P., Claessen, G., Sørensen, E., Mitchell, A., Sellevold, A. B., Enger, S., Onarheim, S., Letnes, J. M., Miljoen, H., Tveit, A., La Gerche, A., & Myrstad, M. (2023). Effects of training adaption in endurance athletes with atrial fibrillation: protocol for a multicentre randomised controlled trial. BMJ Open Sport & Exercise Medicine, 9(2), e001541.
Gevaert, A. B., Böhm, B., Hartmann, H., Goovaerts, I., Stoop, T., Van De Heyning, C. M., Böhm, B., Hartmann, H., Goovaerts, I., Stoop, T., Van de Heyning, C. M., Beckers, P. J., Baldassarri, F., Mueller, S., Oberhoffer, R., Duvinage, A., Haykowsky, M. J., Wisløff, U., Adams, V., Pieske, B., Halle, M., & Van Craenenbroeck, E. M. (2023). Effect of Training on Vascular Function and Repair in Heart Failure With Preserved Ejection Fraction. JACC: Heart Failure.
Eriksen-Volnes T., Grue J., Hellum Olaisen S., Letnes, J. M., Nes, B., Løvstakken, L., Wisløff, U., & Dalen, H. (2023) Normalized Echocardiographic Values From Guideline-Directed Dedicated Views for Cardiac Dimensions and Left Ventricular Function. JACC: Cardiovascular Imaging.
Letnes, J. M., Nes, B. M., & Wisløff, U. (2023). Age-related decline in peak oxygen uptake: Cross-sectional vs. longitudinal findings. A review. International Journal of Cardiology Cardiovascular Risk and Prevention, 16, 200171.
Reitlo, L. S., Mihailovic, J. M., Stensvold, D., Wisløff, U., Hyder, F., & Håberg, A. K. (2023). Hippocampal neurochemicals are associated with exercise group and intensity, psychological health, and general cognition in older adults. GeroScience, 1-19.
2022:
Vesterbekkmo, E. K., Aamot Aksetøy, I. L., Follestad, T., Nilsen, H. O., Hegbom, K., Wisløff, U., Wiseth, R., & Madssen, E. (2022). High intensity interval training induces beneficial effects on coronary atheromatous plaques–a randomized trial. European Journal of Preventive Cardiology.
Keating, S. E., Croci, I., Wallen, M. P., Cox, E. R., Thuzar, M., Pham, U., Mielke, G. I., Coombes, J. S., MacDonald, G. A., & Hickman, I. J. (2022). High-Intensity Interval Training is Safe, Feasible and Efficacious in Nonalcoholic Steatohepatitis: A Randomized Controlled Trial. Digestive Diseases and Sciences, 1-17.
Oldervoll, L. M., Gjestad, R., Hilmarsen C, C., Ose, A., Gullikstad, L., Wisløff, U., Kulseng, B., & Grimsmo, J. (2022). Diastolic function and cardiovascular risk among patients with severe obesity referred to a lifestyle-program–a pilot study. Scandinavian Cardiovascular Journal, 57(1), 8-16.
Johansen, K. R., Ranhoff, A. H., Sørensen, E., Nes, B. M., Heitmann, K. A., Apelland, T., Sandbakk, S. B., Wilsgaard, T., Løchen, M.-L., Thelle, D. S., Morseth, B., & Myrstad, M. (2022). Risk of atrial fibrillation and stroke among older men exposed to prolonged endurance sport practice: a 10-year follow-up. The Birkebeiner Ageing Study and the Tromsø Study. Open Heart, 9(2), e002154.
Sæther, J. C., Klevjer, M., Giskeødegård, G. F., Bathen, T. F., Gigante, B., Gjære, S., Myhra, M., Vesterbekkmo, E. K., Wiseth, R., Madssen, E., & Bye, A. (2022). Small LDL subfractions are associated with coronary atherosclerosis despite no differences in conventional lipids. Physiological Genomics.
Hammer, P., Tari, A. R., Franklin, B. A., Wen, C.-P., Wisløff, U., & Nauman, J. (2022). Personal Activity Intelligence and Ischemic Heart Disease in a Healthy Population: China Kadoorie Biobank Study. Journal of Clinical Medicine.
Aakerøy, L., Cheng, C. W., Sustova, P., Scrimgeour, N. R., Wahl, S. G. F., Steinshamn, S., Bowen, T. S., & Brønstad, E. (2022). Identification of exercise‐regulated genes in mice exposed to cigarette smoke. Physiological Reports, 10(21), e15505.
Zanaboni, P., Manskow, U. S., Sagelv, E. H., Morseth, B., Edvardsen, A. E., Aamot, I.-L., Nes, B. M., Hastings, B., Gagnon, M.-P., & Antypas, K. (2022). Digital interventions to promote physical activity among inactive adults: A study protocol for a hybrid type I effectiveness-implementation randomized controlled trial. Frontiers in Public Health
Benegiamo, G., Bou Sleiman, M., Wohlwend, M., Rodríguez-López, S., Goeminne, L. J., Laurila, P. P., Kleiver, M., Salonen, M. K., Lahti, J., Jha, P., Cogliati, S., Enriquez, J. A., Brumpton, B. M., Bye, A., Eriksson, J. G.,& Auwerx, J. (2022). COX7A2L genetic variants determine cardiorespiratory fitness in mice and human. Nature Metabolism, 1-16.
Winzer, E. B., Augstein, A., Schauer, A., Mueller, S., Fischer-Schaepmann, T., Goto, K., Hommel, J., van Craenenbroeck, E. M., Wisløff, U., Pieske, B., Halle, M., Linke, A., & Adams, V. (2022). Impact of Different Training Modalities on Molecular Alterations in Skeletal Muscle of Patients With Heart Failure With Preserved Ejection Fraction: A Substudy of the OptimEx Trial. Circulation: Heart Failure, 10-1161.
Loe, H., Mosti, M. P., Wisløff, U., Haberstroh, C., & Flemmen, G. (2022). Cardiopulmonary and muscular effects of different doses of high-intensity physical training in substance use disorder patients: study protocol for a block allocated controlled endurance and strength training trial in an inpatient setting. BMJ Open, 12(9), e061014.
Ingul, C. B., Edvardsen, A., Follestad, T., Trebinjac, D., Ankerstjerne, O. A. W., Brønstad, E., Rasch-Halvorsen, Ø., Aarli, B., Dalen, H., Nes, B. M., Lerum, T. V., Einvik, G., Staven, & Skjørten, I. (2022). Changes in cardiopulmonary exercise capacity and limitations 3 to 12 months after COVID-19. European Respiratory Journal.
Tari, A. R., Berg, H. H., Videm, V., Bråthen, G., White, L. R., Røsbjørgen, R. N., Scheffler, K., Dalen, H., Holte, E., Håberg, A. K., Selbæk, G., Lydersen, S., Duezel, E., Bergh, S., Logan-Halvorstud, K. R., Sando, S. B., & Wisløff, U. (2022). Safety and efficacy of plasma transfusion from exercise-trained donors in patients with early Alzheimer’s disease: protocol for the ExPlas study. BMJ Open, 12(9), e056964.
Halle, M., Prescott, E., Van Craenenbroeck, E. M., Beckers, P., Videm, V., Karlsen, T., Feiereisen, P., Winzer, E. B., Mangner, N., Snoer, M., Christle, J. W., Dalen, H., Støylen, A., Esefeld, K., Heitkamp, M., Spanier, B., Linke, A., Ellingsen, Ø., & SMARTEX-HF Study Group. (2022). Moderate continuous or high intensity interval exercise in heart failure with reduced ejection fraction: Differences between ischemic and non-ischemic etiology. American Heart Journal Plus: Cardiology Research and Practice, 100202.
Tauschek, L., Røsbjørgen, R. E., Dalen, H., Larsen, T., & Karlsen, T. (2022). No Effect of Calanus Oil on Maximal Oxygen Uptake in Healthy Participants: A Randomized Controlled Study. International Journal of Sport Nutrition and Exercise Metabolism, 1(aop), 1-11.
Tari, A. R., Selbæk, G., Franklin, B. A., Bergh, S., Skjellegrind, H., Sallis, R. E., Bosnes, I., Stordal, E., Ziaei, M., Lydersen, S., Kobro-Flatmoen, A., Huuha, A. M., Nauman, J., & Wisløff, U. (2022). Temporal changes in personal activity intelligence and the risk of incident dementia and dementia related mortality: A prospective cohort study (HUNT). eClinicalMedicine, 52, 101607.
Carlsen, T., Stensvold, D., Wisløff, U., Ernstsen, L., & Halvorsen, T. (2022). The association of change in peak oxygen uptake with use of psychotropics in community-dwelling older adults-The Generation 100 study. BMC geriatrics, 22(1), 1-10.
Sowa, P. W., Winzer, E. B., Hommel, J., Männel, A., van Craenenbroeck, E. M., Wisløff, U., Pieske, B., Helle, M., Linke, A., & Adams, V. (2022). Impact of different training modalities on high‐density lipoprotein function in HFpEF patients: a substudy of the OptimEx trial. ESC Heart Failure.
Pani, J., Eikenes, L., Reitlo, L. S., Stensvold, D., Wisløff, U., & Håberg, A. K. (2022). Effects of a 5-Year Exercise Intervention on White Matter Microstructural Organization in Older Adults. A Generation 100 Substudy. Frontiers in Aging Neuroscience.
Langlo, K. A. R., Lundgren, K. M., Zanaboni, P., Mo, R., Ellingsen, Ø., Hallan, S. I., Aksetøy, I.-L. A., & Dalen, H. (2022). Cardiorenal syndrome and the association with fitness: Data from a telerehabilitation randomized clinical trial. ESC Heart Failure.
Ness, H. O., Ljones, K., Gjelsvik, R. H., Tjønna, A. E., Malmo, V., Nilsen, H. O., Hollekim-Strand, S. M., Dalen, H., & Høydal, M. A. (2022). Acute effects of high intensity training on cardiac function: a pilot study comparing subjects with type 2 diabetes to healthy controls. Scientific reports, 12(1), 1-11.
Vesterbekkmo, E. K., Madssen, E., Aamot Aksetøy, I. L., Follestad, T., Nilsen, H. O., Hegbom, K., Wisløff, U., & Wiseth, R. (2022). CENIT (impact of cardiac exercise training on lipid content in coronary atheromatous plaques evaluated by near‐infrared spectroscopy): a randomized trial. Journal of the American Heart Association, e024705.
Klevjer, M., Nordeidet, A. N., Hansen, A. F., Madssen, E., Wisløff, U., Brumpton, B. M., & Bye, A. Genome-wide Association Study Identifies New Genetic Determinants of Cardiorespiratory Fitness: The HUNT Study. Medicine and science in sports and exercise.
Pani, J., Marzi, C., Stensvold, D., Wisløff, U., Håberg, A. K., & Diciotti, S. (2022). Longitudinal study of the effect of a 5-year exercise intervention on structural brain complexity in older adults. A Generation 100 substudy. NeuroImage, 119226.
Smenes, B. T., Nes, B. M., Letnes, J. M., Slagsvold, K. H., Wisløff, U., Wahba, A. (2022). Cardiorespiratory fitness and the incidence of coronary surgery and postoperative mortality: the HUNT study. European Journal of Cardio-Thoracic Surgery.
Taraldsen, M. D., Wiseth, R., Videm, V., Bye, A., & Madssen, E. (2022). Associations between circulating microRNAs and coronary plaque characteristics: potential impact from physical exercise. Physiological Genomics.
Ingul, C. B., Grimsmo, J., Mecinaj, A., Trebinjac, D., Berger Nossen, M., Andrup, S., Grenne, B., Dalen, H., Einvik, G., Stavem, K., Follestad, T:, Josefsen, T., Omland , T., & Jensen, T. (2022). Cardiac Dysfunction and Arrhythmias 3 Months After Hospitalization for COVID‐19. Journal of the American Heart Association, e023473.
Nodeland, M., Klevjer, M., Sæther, J., Giskeødegård, G., Bathen, T. F., Wisløff, U., & Bye, A. (2022). Atherogenic lipidomics profile in healthy individuals with low cardiorespiratory fitness: The HUNT3 fitness study. Atherosclerosis
Arild, A., Vangberg, T., Nikkels, H., Lydersen, S., Wisløff, U., Stensvold, S., & Håberg, A. K., (2022). Five years of exercise intervention at different intensities and development of white matter hyperintensities in community dwelling older adults, a Generation 100 sub-study. Aging.
Huuha, A. M., Norevik, C. S., Moreira, J. B. N., Kobro-Flatmoen, A., Scrimgeour, N., Kivipelto, M., van Praag, H., Ziaei, M., Sando, S. B., Wisløff, U., & Tari, A. R. (2022). Can Exercise Training Teach Us How to Treat Alzheimer’s disease?. Ageing Research Reviews, 101559.
2021:
Wohlwend, M., Laurila, P.-P., Williams, K., Romani, M, Lima, T., Pattawaran, P., Benegiamo, G., Salonen, M., Schneider, B., Lahti, J., Eriksson, J. G., Barrés, R., Wisløff, U., Moreira, J. B. N., & Auwerx, J. (2021). The exercise-induced long noncoding RNA CYTOR promotes fast-twitch myogenesis in aging. Science Translational Medicine, 13(623), eabc7367
Zotcheva, E., Håberg, A. K., Wisløff, U., Salvesen, Ø., Selbæk,. G., Stensvold, D., & Erntsen, L. (2021). Effects of 5 Years Aerobic Exercise on Cognition in Older Adults: The Generation 100 Study: A Randomized Controlled Trial. Sports Medicine, 1-11
Nauman, J., Franklin, B. A., Nes, B. M., Sallis, R. E., Sawada, S. S., Marinovic, J., Stensvold, D., Lavie, C. J., Tari, A. R., & Wisløff, U. (2021) Association Between Personal Activity Intelligence and Mortality: Population-Based China Kadoorie Biobank Study. Mayo Clinic Proceedings
Sokolowski, D. R., Hansen, I. T., RIsen, H. H., Reitlo, L. S., Wisløff, U., Stensvold, D., & Håberg, A. K. (2021). 5 Years of Exercise Intervention Did Not Benefit Cognition Compared to the Physical Activity Guidelines in Older Adults, but Higher Cardiorespiratory Fitness Did. A Generation 100 Substudy. Frontiers in Aging Neuroscience
Letnes, J. M., Berglund, I., Johnson, K. E., Dalen, H., Nes, B. M., Lydersen, S., Viken, H., Hassel, E., Steinshamn, S., Vesterbekkmo, E. K., Støylen, A., Reitlo, L. S., Zisko, N., Bækkerud, F. H., Tari, A. R., Ingebrigtsen, J. E., Sandbakk, S. B., Carlsen, T., Anderssen, S. A., Singh, M. A. F., Coombes, J. S., Helbostad, J. L., Rognmo, Ø., Wisløff, U., & Stensvold, D. (2021) Effect of 5 years of exercise training on the cardiovascular risk profile of older adults: the Generation 100 randomized trial. European Heart Journal, ehab721
Aakerøy, L., Nørstebø, E. A., Thomas, K. M., Holte, E., Hegbom, K., Brønstad, E., & Steinshamn, S. (2021). High-intensity interval training and pulmonary hemodynamics in COPD with hypoxemia. European Clinical Respiratory Journal, 8(1), 1984642.
Alrahma, A. M., Habib, M. A., Oulhaj, A., Loney, T., Boillat, T., Shah, S. M., Ahmed, L. A., & Nauman, J. (2021). Effects of a workplace exercise intervention on cardiometabolic health: study protocol for a randomised controlled trial. BMJ Open, 11(11):e051070
Berglund, I., Vesterbekkmo, E. K., Retterstøl, K., Anderssen, S. A., Singh, M. A. F., Helge, J. W., Lydersen, S., Wisløff, U., & Stensvold, D. (2021). The Long-term Effect of Different Exercise Intensities on High-Density Lipoprotein Cholesterol in Older Men and Women Using the Per Protocol Approach: The Generation 100 Study. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 5(5), 859-871.
Gevaert, A. B., Witvrouwen, I., Van Craenenbroeck, A. H., Van Laere, S. J., Boen, J. R., Van de Heyning, C. M., Belyavskiy, E., Mueller, S., Winzer, E., Duvinage, A., Edelmann, F., Beckers, P. J., Heidbuchel, H., Wisløff, U., Pieske, B., Adams, V., Halle, M., Van Craenenbroeck, E., & OptimEx-Clin Study Group. (2021). miR-181c level predicts response to exercise training in patients with heart failure and preserved ejection fraction: an analysis of the OptimEx-Clin trial. European Journal of Preventive Cardiology.
Skjørten, I., Ankerstjerne, O. A. W., Trebinjac, D., Brønstad, E., Rasch-Halvorsen, Ø., Einvik, G., Lerum, T. V., Stavem, K., & Ingul, C. B. (2021). Cardiopulmonary exercise capacity and limitations 3 months after COVID-19 hospitalisation. European Respiratory Journal, 58(2).
Pani, J., Reitlo, L. S., Evensmoen, H. R., Lydersen, S., Wisløff, U., Stensvold, D., & Håberg, A. K. (2021). Effect of 5 Years of Exercise Intervention at Different Intensities on Brain Structure in Older Adults from the General Population: A Generation 100 Substudy. Clinical Interventions in Aging, 16, 1485-1501.
Gunnes, M., Aksetøy, I. L. A., Follestad, T., Indredavik, B., & Askim, T. (2021). Can functional walk tests add value to the prediction of cardiorespiratory fitness after stroke? A prospective cohort study. Plos one, 16(8), e0255308.
Miguel-dos-Santos, R., Moreira, J. B. N., Loennechen, J. P., Wisløff, U., & Mesquita, T. (2021). Exercising immune cells: The immunomodulatory role of exercise on atrial fibrillation. Progress in Cardiovascular Diseases.
Gjellesvik, T. I., Becker, F., Tjønna, A. E., Indredavik, B., Lundgaard, E., Solbakken, H., Brurok, B., Tørhaug, T., Lydersen, S., & Askim, T. (2021). Effects of High-Intensity Interval Training after Stroke (The HIIT Stroke Study) on Physical and Cognitive Function: A Multicenter Randomized Controlled Trial: Treadmill interval training after stroke. Archives of Physical Medicine and Rehabilitation.
Aandahl, M. H., Noordhof, D. A., Tjønna, A. E., & Sandbakk, Ø. (2021). Effect of Carbohydrate Content in a Pre-event Meal on Endurance Performance-Determining Factors: A Randomized Controlled Crossover-Trial. Frontiers in Sports and Active Living, 3.
Rasch-Halvorsen, Ø., Hassel, E., Brumpton, B. M., Jenssen, H., Spruit, M. A., Langhammer, A., & Steinshamn, S. (2021). Lung function and peak oxygen uptake in chronic obstructive pulmonary disease phenotypes with and without emphysema. PloS one, 16(5), e0252386.
Williams, C. J., Li, Z., Harvey, N., Lea, R. A., Gurd, B. J., Bonafiglia, J. T., Papadimitrou, I., Jacques, M., Croci, I., Stensvold, D., Wisløff, U., Taylor, J. L., Gajanand, T., Cox, E. R., Ramos, J. S., Fassett, R. B., Little, J. P., Francois, M. E., Hearon Jr, C. M., Sarma, S., Janssen, S. L. J. E., van Craenenbroeck, E. M., Beckers, P., Cornelissen, V. A., Howden, E. J., Keating, S. E., Yan, X., Bishop, D. J., Bye, A., Haupt, L. M., Griffiths, L. R., Ashton, K. J., Brown, M. A., Torquati, L., Eynon; N., & Coombes, J. S. (2021). Genome wide association study of response to interval and continuous exercise training: the Predict-HIIT study. Journal of Biomedical Science, 28(1), 1-15.
Letnes, J. M., Eriksen-Volnes, T., Nes, B., Wisløff, U., Salvesen, Ø., & Dalen, H. Variability of echocardiographic measures of left ventricular diastolic function. The HUNT study. Echocardiography (Mount Kisco, NY).
Adams, V., Wunderlich, S., Mangner, N., Hommel, J., Esefeld, K., Gielen, S., Halle, M., Ellingsen, Ø., van Craenenbroeck, E., Wisløff, U., Pieske, B., Linke, A., & Winzer, E. B. (2021). Ubiquitin-proteasome-system and enzymes of energy metabolism in skeletal muscle of patients with HFpEF and HFrEF. ESC Heart Failure
de Souza, R. W. A., Gallo, D., Lee, G. R., Katsuyama, E., Schaufler, A., Weber, J., Csizmadia, E., Tsokos, G. C., Koch, L. G., Britton, S. L., Wisløff, U., Brum, P. C. & Otterbein, L. E. (2021). Skeletal muscle heme oxygenase-1 activity regulates aerobic capacity. Cell Reports, 35(3), 109018.
Ghram, A., Jenab, Y., Soori, R., Choobineh, S., Hosseinsabet, A., Niyazi, S., Shirani, S., Shafiie, A., & Wisløff, U. (2021). High-Intensity Interval Training in Patients with Pulmonary Embolism: A Randomized Controlled Trial. Medicine and Science in Sports and Exercise.
Lundgren, K. M., Aspvik, N. P., Langlo, K. A. R., Braaten, T., Wisløff, U., Stensvold, D., & Karlsen, T. (2021). Blood Volume, Hemoglobin Mass, and Peak Oxygen Uptake in Older Adults: The Generation 100 Study. Frontiers in Sports and Active Living.
Rutkovskiy, A., Lyngbakken, M. N., Dahl, M. B., Bye, A., Pedersen, M. H., Wisløff, U., Christensen, G., Høiseth, A. D., Omland, T., & Røsjø, H. (2021). Circulating MicroRNA-210 Concentrations in Patients with Acute Heart Failure: Data from the Akershus Cardiac Examination 2 Study. Clinical Chemistry.
Bode, D., Rolim, N. P. L., Guthof, T., Hegemann, N., Wakula, P., Primessnig, U., Berre, A. M. O., Adams, V., Wisløff, U., Pieske, B. M., Heinzel, F. R., Hohendanner, F., & OptimEx Study Group (2021). Effects of different exercise modalities on cardiac dysfunction in heart failure with preserved ejection fraction. ESC Heart Failure.
Koppen, E., Omland, T., Larsen, A. I., Karlsen, T., Linke, A., Prescott, E., Halle, M., Dalen, H., Delagardelle, C., Hole, T., van Craenenbroeck, E. M., Beckers, P., Ellingsen, Ø., Feiereisen, P., Valborgland, T., Videm, V., & SMARTEX-HF Study Group. Exercise training and high-sensitivity cardiac troponin T in patients with heart failure with reduced ejection fraction. ESC Heart Failure.
Kieffer, S. K., Nauman, J., WSyverud, K., Selboskar, H., Lydersen, S., Ekelund, U., & Wisløff, U. (2021). Association between Personal Activity Intelligence (PAI) and body weight in a population free from cardiovascular disease – The HUNT study. The Lancet Regional Health Europe
Liff, M. H., Hoff, M., Wisløff, U., & Videm, V. (2021). Reduced cardiorespiratory fitness is a mediator of excess all-cause mortality in rheumatoid arthritis: the Trøndelag Health Study. RMD Open, 7(1):e001545
Langlo, K. A. R., Silva, G. J. J., Overrein, T. S., Adams, V., Wisløff, U., Dalen, H., Rolim, N. & Hallan, S. I. (2021). Circulating microRNAs May Serve as Biomarkers for Hypertensive Emergency End-Organ Injuries and Address Underlying Pathways in an Animal Model. Frontiers in cardiovascular medicine, 7, 626699.
Mueller, S., Winzer, E. B., Duvinage, A., Gevaert, A. B., Edelmann, F., Haller, B., Pieske-Kraigher, E., Beckers, P., Bobenko, A., Hommel, J., Van de Heyning, C. M., Esefeld, K., von Korn, P., Christle, J. W., Haykowsky, M. J., Linke, A., Wisløff, U., Adams, V., Pieske, B., can Craenenbrock, E., & Halle, M. (2021). Effect of High-Intensity Interval Training, Moderate Continuous Training, or Guideline-Based Physical Activity Advice on Peak Oxygen Consumption in Patients With Heart Failure With Preserved Ejection Fraction: A Randomized Clinical Trial. JAMA, 325(6), 542-551.
Way, K., Vidal-Almela, S., Moholdt, T., Currie, K. D., Aksetøy, I.-L. A., Boidin, M., Cornelissen, V. A., Joa, K., Keech, A., Jayo-Montoya, J. A., Taylor, J. L., Fouriner, K., & Reed, J. L. (2021). Sex differences in Cardiometabolic Health Indicators following HIIT in Patients with Coronary Artery Disease. Medicine & Science in Sports & Exercise
2020:
Nauman, J., Arena, R., Zisko, N., Sui, X., Lavie, C. J., Laukkanen, J. A., Blair, S. N., Dunn, P., Nes, B. M., Tari, A. R., Stensvold, D., Whitsel, L. P., & Wisløff, U. (2020). Temporal changes in personal activity intelligence and mortality: Data from the aerobics center longitudinal study. Progress in Cardiovascular Diseases.
Goto, K., Schauer, A., Augstein, A., Methawasin, M., Granzier, H., Halle, M., van Craenenbroeck, E. M., Rolim, N., Gielen, S., Pieske, B., Winzer, E. B., Linke, A., & Adams, V. (2021). Muscular changes in animal models of heart failure with preserved ejection fraction: what comes closest to the patient?. ESC heart failure, 8(1), 139-150.
D'Souza, A., Wang, Y., Anderson, C., Bucchi, A., Barsucotti, M., Olieslagers, S., Mesirca, P., Johnsen, A. B., Masitskaya, S., Ni, H., Zhang, Y., Black, N., Cox, C., Wegner, S., Bano-Otalora, B., Petit, C., Gill, E:, Logantha, S. J., Dobrzynski, H., Ashton, N., Hart, G., Zhang, R., Zhang, H., Cartwright, E. J., Wisløff, U., Mangoni, M. E., Martins, P. D. C., Piggins, H. D., DiFrancesco, D., & Boyett, M. R. (2020). A circadian clock in the sinus node mediates day-night rhythms in Hcn4 and heart rate. Heart Rhythm
von Korn, P., Keating, S., Mueller, S., Haller, B., Kraenkel, N., Dinges, S., Duvinage, A., Scherr, J., Wisløff, U., Tjønna, A. E., Halle, M., & Lechner, K. (2020). The Effect of Exercise Intensity and Volume on Metabolic Phenotype in Patients with Metabolic Syndrome: A Randomized Controlled Trial. Metabolic Syndrome and Related Disorders.
Mehta, A., Kondamudi, N., Laukkanen, J. A., Wisloff, U., Franklin, B. A., Arena, R., Lavie, C. J., & Pandey, A. (2020). Running away from cardiovascular disease at the right speed: The impact of aerobic physical activity and cardiorespiratory fitness on cardiovascular disease risk and associated subclinical phenotypes. Progress in Cardiovascular Diseases.
Liff, M. H., Hoff, M., Wisløff, U., & Videm, V. (2020). Faster age-related decline in cardiorespiratory fitness in rheumatoid arthritis patients: an observational study in the Trøndelag Health Study. Rheumatology International, 1-11.
Stensvold, D., Viken, H., Steinshamn, S. L., Dalen, H., Støylen, A., Loennechen, J. P., Reitlo, L. S., Zisko, N., Bækkerud, F. H., Tari, A., Sandbakk, S. B., Carlsen, T., Ingebrigtsen, J. E., Lydersen, S., Mattsson, E., Anderssen, S. A., Singh, M. A. F., Coombes, J. S., Skogvoll, E., Vatten, L. J., Helbostad, J. L., Rognmo, Ø., & Wisløff, U. (2020) Effect of exercise training for five years on all cause mortality in older adults—the Generation 100 study: randomised controlled trial. The BMJ
Letnes, J. M., Dalen, H., Aspenes, S. T., Salvesen, Ø., Wisløff, U., & Nes, B. M. (2020) Age-related change in peak oxygen uptake and change of cardiovascular risk factors. The HUNT Study. Progress in Cardiovascular Diseases.
Stølen, T. O., Høydal, M. A., Ahmed, M. S., Jørgensen, K., Garten, K., Hortigon-Vinagre, M. P., Zamora, V., Scrimgeour, N. R., Berre, A. M. O., Nes, B. M., Skogvoll, E., Moreira, J. B., McMullen, J. R., Attramadal, H., Smith, G. L., Ellingsen, Ø., & Wisløff, U. (2020). Exercise training reveals micro-RNAs associated with improved cardiac function and electrophysiology in rats with heart failure after myocardial infarction. Journal of Molecular and Cellular Cardiology.
Rodrigues, J. A. L., Stenvold, D., Almeida, M. L., Sobrinho, A. C. S., Rodrigues, G. S., & Júnior, C. R. (2020). Cardiometabolic risk factors associated with educational level in older people: comparison between Norway and Brazil. Journal of Public Health.
Moreira, J. B., Wohlwend, M., & Wisløff, U. (2020) Exercise and cardiac health: physiological and molecular insights. Nature Metabolism, 1-11
Mallard, A. R., Hollekim-Strand, S. M., Ingul, C. B., & Coombes, J. S. (2020). High day-to-day and diurnal variability of oxidative stress and inflammation biomarkers in people with type 2 diabetes mellitus and healthy individuals. Redox Report, 25(1), 64-69.
Moreira, J. B., & Wisløff, U. (2020). Post-exercise breast milk: the new polypill?. Nature Metabolism, 1-2.
Nauman, J., Sui, X., Lavie, C. J., Wen, C. P., Laukkanen, J. A., Blair, S. N., Dunn, P., Arena, R., & Wisløff, U. (2020). Personal activity intelligence and mortality – Data from the Aerobics Center Longitudinal Study. Progress in Cardiovascular Diseases.
Lund, J. S., Aksetøy, I. L. A., Dalen, H., Amundsen, B. H., & Støylen, A. (2020). Left ventricular diastolic function: Effects of high‐intensity exercise after acute myocardial infarction. Echocardiography.
Alves, C., Neves, W. D., de Almeida, N. R., Eichelberger, E. J., Jannig, P. R., Voltarelli, V. A., Tobias, G. C., Bechara, L., de P Faria, D., Alves, M., Hagen, L., Sharma, A., Slupphaug, G., Moreira, J., Wisloff, U., Hirshman, M. F., Negrão, C. E., de Castro, G., Jr, Chammas, R., Swoboda, K. J., Ruas, J. L., Goodyear, L. J., Brum, P. C. (2020). Exercise training reverses cancer-induced oxidative stress and decrease in muscle COPS2/TRIP15/ALIEN. Molecular metabolism, 101012.
Rasch-Halvorsen, Ø., Hassel, E., Brumpton, B. M., Jenssen, H., Spruit, M. A., Langhammer, A., & Steinshamn, S. (2020). The association between normal lung function and peak oxygen uptake in patients with exercise intolerance and coronary artery disease. PloS one, 15(5), e0232693.
Calverley, T. A., Ogoh, S., Marley, C. J., Steggall, M., Marchi, N., Brassard, P., Lucas, S. J. E., Cotter, J. D:, Roig, M., Ainslie, P. N, Wisløff, U., & Bailey, D. M. (2020). HIITing the brain with exercise; mechanisms, consequences and practical recommendations. The Journal of Physiology.
Weston, K., Barker, A. R., Bond, B., Costigan, S., Ingul, C., & Williams, C. (2020). The BASES Expert Statement on the Role of High-intensity Interval Exercise for Health and Fitness Promotion in Young People. The Sport and Exercise Scientist, (64), 8-9.
Halle, K. K., Bakke, Ø., Djurovic, S., Bye, A., Ryeng, E., Wisløff, U., Andreassen, O. A., & Langaas, M. (2020): Computationally efficient familywise error rate control in genome‐wide association studies using score tests for generalized linear models. Scandinavian Journal of Statistics.
Taraldsen, M. D., Videm, V., Hegbom, K., Wiseth, R., & Madssen, E. (2020). Stent edge vascular response and in-stent geometry after aerobic exercise. Cardiovascular Intervention and Therapeutics, 1-10.
Gjellesvik, T. I., Becker, F., Tjønna, A. E., Indredavik, B., Nilsen, H., Brurok, B., Tørhaug, T., Busuladzic, M., Lydersen, S., & Askim, T. (2020). Effects of High-Intensity Interval Training after Stroke (The HIIT-Stroke study)-A Multicenter Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation.
Ghram, A., Shafiee, A., Soori, R., Choobineh, S., Niyazi, S., Shirani, S., Hosseinsabet, A., Wisløff, U., & Jenab, Y. (2020). Safety and efficacy of high intensity interval training in a patient with acute pulmonary embolism. Progress in Cardiovascular Diseases.
Garnvik, L. E., Malmo, V., Jansky, I., Ellekjær, H., Wisløff, U., Loennechen, J. P., & Nes, B. (2020). Physical activity, cardiorespiratory fitness, and cardiovascular outcomes in individuals with atrial fibrillation: the HUNT study. European Heart Journal. ehaa032
Bye, A., Klevjer, M., Ryeng, E., Silva, G. J., Moreira, J. B. N., Stensvold, D., & Wisløff, U. (2020). Identification of novel genetic variants associated with cardiorespiratory fitness. Progress in Cardiovascular Diseases.
Gigante, B., Papa, L., Bye, A., Kunderfranco, P., Viviani, C., Roncarati, R., Briguori, C., de Faire, U., Bottai, M., & Condorelli, G. (2020). MicroRNA signatures predict early major coronary events in middle-aged men and women. Cell death & disease, 11(1), 1-3.
Letnes, J. M., Nes, B. N., Vaardal-Lunde, K., Slette, M. B., Mølmen-Hansen, H. E., Aspenes, S. T., Støylen, A., Wisløff, U., & Dalen, H. (2020). Left Atrial Volume, Cardiorespiratory Fitness, and Diastolic Function in Healthy Individuals: The HUNT Study, Norway. Journal of the American Heart Association, 9(3), e014682
Liff, M. H., Hoff, M., Fremo, T., Wisløff, U., & Videm, V. (2020). An Estimation Model for Cardiorespiratory Fitness in Adults with Rheumatoid Arthritis. Medicine & Science in Sports & Exercise
Rodrigues, J. A. L., Ferrari, G. D., Trapé, Á. A., de Moraes, V. N., Gonçalves, T. C. P., Tavares, S. S., Tjønna, A. E., de Souza, H. C. D., & Júnior, C. R. B. (2020). β 2 adrenergic interaction and cardiac autonomic function: effects of aerobic training in overweight/obese individuals. European Journal of Applied Physiology, 120(3), 613-624.
2019:
Peterman, J. E., Arena, R., Myers, J., Marzolini, S., Ross, R., Lavie, C. J., Wisløff, U., Stensvold, D., & Kaminsky, L. A. (2019). Development of Global Reference Standards for Directly Measured Cardiorespiratory Fitness: A Report From the Fitness Registry and Importance of Exercise National Database (FRIEND). Mayo Clinic Proceedings
Nauman, J., Khan, M. A., & Joyner, M. J. (2019). Walking in the Fast Lane: High-Intensity Walking for Improved Fitness and Health Outcomes. In Mayo Clinic Proceedings, 94(12), 2378-2380
Arena, R., Myers, J., Harber, M., Wisløff, U., Stensvold, D., & Kaminsky, L. (2019). Peak oxygen pulse responses during maximal cardiopulmonary exercise testing: Reference standards from FRIEND (Fitness Registry and the Importance of Exercise: an International Database). International Journal of Cardiology.
Dias, K. A., Ramos, J. S., Wallen, M. P., Davies, P. S., Cain, P. A., Leong, G. M., Ingul, C. B., Coombes, J. S., & Keating, S. E. (2019). Accuracy of Longitudinal Assessment of Visceral Adipose Tissue by Dual-Energy X-Ray Absorptiometry in Children with Obesity. Journal of Obesity, 2019.
Karlsen, T., Videm, V., Halle, M., Ellingsen, Ø., Støylen, A., Dalen, H., Dalgardelle, C., Larsen, A. I., Hole, T., Mezzani, A., van Crenenbroeck, E. M., Beckers, P., Pressler, A., Christle, J. W., Winzer, E., Mangner, N., Woitek, F., Höllriegel, R., Snoer, M., Feiereisen, P., Valborgland, T., Linke, A., & Prescott, E. (2019). Baseline and Exercise Predictors of VO2peak in Systolic Heart Failure Patients: Results from SMARTEX-HF. Medicine and science in sports and exercise.
Tari, A. R., Nauman, J., Zisko, N., Skjellegrind, H. K., Bosnes, I., Bergh, S., Stensvold, D., Selbæk, G., & Wisløff, U. (2019). Temporal changes in cardiorespiratory fitness and risk of dementia incidence and mortality: a population-based prospective cohort study. The Lancet Public Health, 4(11), e565-e574.
Stølen, T., Shi, M., Wohlwend, M., Høydal, M. A., Bathen, T. F., Ellingsen, Ø., & Esmaeili, M. (2019). Effect of exercise training on cardiac metabolism in rats with heart failure. Scandinavian Cardiovascular Journal, 1-8.
Laukkanen, J. A., Kunutsor, S. K., Ozemek, C., Mäkikallio, T., Lee, D. C., Wisloff, U., & Lavie, C. J. (2019). Cross-country skiing and running's association with cardiovascular events and all-cause mortality: A review of the evidence. Progress in Cardiovascular Diseases.
Velle-Forbord, T., Eidlaug, M., Debik, J., Sæther, J. C., Follestad, T., Nauman, J., Gigante, B., Røsjø, H., Omland, T., Langaas, M., & Bye, A. (2019). Circulating microRNAs as predictive biomarkers of myocardial infarction: Evidence from the HUNT study. Atherosclerosis.
Garnvik, L. E., Malmo, V., Janszky, I., Wisløff, U., Loennechen, J. P., & Nes, B. M. (2019). Estimated Cardiorespiratory Fitness and Risk of Atrial Fibrillation: The HUNT Study. Medicine and science in sports and exercise.
Lavie, C. J., Hecht, H. F., & Wisloff, U. (2019). Extreme Physical Activity May Increase Coronary Calcification, But Fitness Still Prevails. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 3(2), 103-105.
Nordstoga, A. L., Zotcheva, E., Svedahl, E. R., Nilsen, T. I. L., & Skarpsno, E. S. (2019). Long-term changes in body weight and physical activity in relation to all-cause and cardiovascular mortality: the HUNT study. International Journal of Behavioral Nutrition and Physical Activity, 16(45)
Liff, M. H., Hoff, M., Fremo, T., Wisløff, U., Thomas, R., & Videm, V. (2019). Cardiorespiratory fitness in patients with rheumatoid arthritis is associated with the patient global assessment but not with objective measurements of disease activity. RMD Open, 5(1), e000912.
Bode, D., Lindnes, D., Schwarz, M., Westermann, D., Deisler, P., Primessnig, U., Hegemann, N., Blatter, L. A., van Linthout, S., Tschöpe, C., Schoenrah, F., Soltani, S, Stamm, C., Duesterhoeft, V., Rolim, N., Wisløff, U., Knosalla, C., Falk, V., Pieske, B. M., Heinzel, F. R., & Hohendanner, F. (2019). The role of fibroblast – Cardiomyocyte interaction for atrial dysfunction in HFpEF and hypertensive heart disease. Journal of Molecular and Cellular Cardiology
Shigdel, R., Dalen, H., Sui, X., Lavie, C. J., Wisløff, U., & Ernstsen, L. (2019). Cardiorespiratory fitness and the risk of first acute myocardial infarction: the HUNT Study. Journal of the American Heart Association, 8(9), e010293.
Pedersen, E. S., Tengesdal, S., Radtke, M., & Rise, K. A. L. (2019). Major increase in creatine kinase after intensive exercise. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke, 139(7).
Berg, J., Undebakke, V., Rasch-Halvorsen, Ø., Aakerøy, L., Sandbakk, Ø., & Tjønna, A. E. (2019). Comparison of mitochondrial respiration in M. triceps brachii and M. vastus lateralis between elite cross-country skiers and physically active controls. Frontiers in Physiology
Madssen, E., Skaug, E. A., Wisløff, U., Ellingsen, Ø., & Videm, V. (2019, March). Inflammation Is Strongly Associated With Cardiorespiratory Fitness, Sex, BMI, and the Metabolic Syndrome in a Self-reported Healthy Population: HUNT3 Fitness Study. Mayo Clinic Proceedings.
Bækkerud, F. H., Salerno, S., Cariotti, P., Morland, C., Storm-Mathisen, J. S., Bergersen, L. H., Høydal, M. A., Catalucci, D., & Stølen, T. O. (2019) High Intensity Interval Training Ameliorates Mitochondrial Dysfunction in the Left Ventricle of Mice with Type 2 Diabetes. Cardiovascular Toxicology
Zotcheva, E., Pintzka, C. W. S., Salvesen, Ø., Selbæk, G., Håberg, A. K., & Ernstsen, L. (2019). Associations of Changes in Cardiorespiratory Fitness and Symptoms of Anxiety and Depression with Brain Volumes: The HUNT Study. Frontiers in Behavioral Neuroscience, 13, 53.
Shi, M., Ellingsen, Ø., Bathen, T. F., Høydal, M. A., Stølen, T., & Esmaeili, M. (2019). The Effect of Exercise Training on Myocardial and Skeletal Muscle Metabolism by MR Spectroscopy in Rats with Heart Failure. Metabolites, 9(3), 53.
Rognmo, Ø., & Wisløff, U. (2019). Exercise in medicine. Progress in cardiovascular diseases.
Moreria, J. B. N., Wohlwend, M., Fenk, S., Åmellem, I., Flatberg, A., Kraljevic, J., Marinovic, J., Ljubkovic, M., Bjørkøy, G., & Wisløff, U. (2019). Exercise reveals proline dehydrogenase as a potential target in heart failure. Progress in Cardiovascular Diseases.
Tari, A. R., Norevik, C. S., Scrimgeour, N. R., Kobro-Flatmoen, A., Storm-Mathisen, J., Bergersen, L. H., Wrann, C. D., Selbæk, G., Kivipelto, M., Moreira, J. B. N., & Wisløff, U. (2019). Are the Neuroprotective Effects of Exercise Training Systemically Mediated?. Progress in Cardiovascular Diseases.
Nauman, J., Nes, B. M., Zisko, N., Revdal, A., Myers, J., Kaminsky, L. A., & Wisløff, U. (2019). Personal activity intelligence (PAI): A new standard in activity tracking for obtaining a healthy cardiorespiratory fitness level and low cardiovascular risk. Progress in Cardiovascular Diseases.
Ozemek, C., Lavie, C. J., & Rognmo, Ø. (2019). Global Physical Activity Levels-Need for Intervention. Progress in Cardiovascular Diseases.
Croci, I., Coombes, J., Sandbakk, S. B., Keating, S. E., Nauman, J., Macdonald, G. A., & Wisløff, U. (2019). Non-alcoholic fatty liver disease: prevalence and all-cause mortality according to sedentary behaviour and cardiorespiratory fitness. The HUNT Study Progress in Cardiovascular Diseases.
Dalen, T., Sandmæl, S., Stevens, T. G., Hjelde, G. H., Kjøsnes, T. N., & Wisløff, U. (2019). Differences in Acceleration and High-Intensity Activities Between Small-Sided Games and Peak Periods of Official Matches in Elite Soccer Players. The Journal of Strength & Conditioning Research.
Undebakke, V., Berg, J., Tjønna, A. E., & Sandbakk, Ø. (2019). Comparison of Physiological and Perceptual Responses to Upper-, Lower-, and Whole-Body Exercise in Elite Cross-Country Skiers. The Journal of Strength & Conditioning Research.
Williams, C. J., Gurd, B. J., Bonafiglia, J. T., Voisin, S. A. C., Li, Z., Harvey, N., Croci, I., Taylor, J. L., Gajanand, T., Ramos, J. S., Fassett, R. G., Little, J. P., Francois, M. E., Hearon Jr., C. M., Sarma, S., Janssen, S. L. J. E., Caenenbroeck, E. M. V., Beckers, P., Cornelissen, V. A., Pattyn, N., Howden, E. K., Keating, S. E., Bye, A., Stensvold, D., Wisløff, U., Papadimitriou, I., Yan, X., Bishop, D. J., Eynon, N., & Coombes, J., (2019). A multi-centre comparison of V̇O2peak trainability between interval training and moderate intensity continuous training. Frontiers in Physiology, 10, 19.
Lavie, C., Wisløff, U., & Blumenthal, R. S. Extreme Physical Activity and Coronary Artery Calcification—Running Heavily and Safely With “Hearts of Stone”. JAMA Cardiology
Taylor, J. L., Holland, D. J., Spathis, J. G., Beetham, K. S., Wisløff, U., Keating, S. E., & Coombes, J. S. (2019). Guidelines for the Delivery and Monitoring of High Intensity Interval Training in Clinical Populations. Progress in Cardiovascular Diseases.
Dalen, T., Lorås, H., Hjelde, G. H., Kjøsnes, T. N., & Wisløff, U. (2019). Accelerations – a new approach to quantify physical performance decline in male elite soccer?. European Journal of Sport Science, 1-9.
Kaminsky, L. A., Arena, R., Ellingsen, Ø., Harber, M. P., Myers, J., Ozemek, C., & Ross, R. (2019). Cardiorespiratory Fitness and Cardiovascular Disease-the Past, Present, and Future. Progress in cardiovascular diseases.
Rasch-Halvorsen, Ø., Hassel, E., Langhammer, A., Brumpton, B. M., & Steinshamn, S. (2019). The association between dynamic lung volume and peak oxygen uptake in a healthy general population: the HUNT study. BMC Pulmonary Medicine, 19(1), 2.
2018:
Souza, R. W., Alves, C. R., Medeiros, A., Rolim, N., Silva, G. J., Moreira, J. B., Alves, M. N., Wohlwend, M., Gebriel, M., Hagen, L., Sharma, A., Koch, L. G., Britton, S. L., Slupphaug, G., Wisløff, U., & Brum, P. C. (2018). Differential regulation of cysteine oxidative post-translational modifications in high and low aerobic capacity. Scientific reports, 8(1), 17772.
Shi, M., Ellingsen, Ø., Bathen, T. F., Høydal, M. A., Koch, L. G., Britton, S. L., Wisløff, U., Stølen, T., & Esmaeili, M. (2018). Skeletal muscle metabolism in rats with low and high intrinsic aerobic capacity: Effect of aging and exercise training. PLOS ONE, 13(12), e0208703.
Letnes, J. M., Dalen, H., Vesterbekkmo, E. K., Wisløff, U., & Nes, B. M. (2018). Peak oxygen uptake and incident coronary heart disease in a healthy population: the HUNT Fitness Study European Heart Journal, ehy708
Berglund, I. J., Sørås, S. E., Relling, B. E., Lundgren, K. M., Kiel, I. A., & Moholdt, T. (2018). The relationship between maximum heart rate in a cardiorespiratory fitness test and in a maximum heart rate test. Journal of Science and Medicine in Sport.
Ozemek, C., Laddu, D. R., Lavie, C. J., Claeys, H., Kaminsky, L. A., Ross, R., Wisløff, U., Arena, R., & Blair, S. N. (2018). An Update on the Role of Cardiorespiratory Fitness, Structured Exercise and Lifestyle Physical Activity in Preventing Cardiovascular Disease and Health Risk. Progress in Cardiovascular Diseases.
Gunnes, M., Langhammer, B., Aamot, I. L., Lydersen, S., Ihle-Hansen, H., Indredavik, B., Kristine H. Reneflot, Schroeter, W., & Askim, T. (2018). Adherence to a Long-Term Physical Activity and Exercise Program After Stroke Applied in a Randomized Controlled Trial. Physical therapy.
Thomsen, R. S., Nilsen, T. I. L., Haugeberg, G., Bye, A., Kavanaugh, A., & Hoff, M. (2018). Effect of high-intensity interval training on cardiovascular disease risk factors and body composition in psoriatic arthritis: a randomised controlled trial. RMD Open, 4(2), e000729.
Zotcheva, E., Bergh, S., Selbæk, G., Krokstad, S., Håberg, A. K., Strand, B. H., & Ernstsen, L. (2018). Midlife Physical Activity, Psychological Distress, and Dementia Risk: The HUNT Study. Journal of Alzheimer's Disease, (Preprint), 1-9.
Tucker, W. J., Beaudry, R. I., Liang, Y., Clark, A. M., Tomczak, C. R., Nelson, M. D., Ellingsen, Ø., & Haykowsky, M. J. (2018). Meta-analysis of exercise training on left ventricular ejection fraction in heart failure with reduced ejection fraction: a 10–year update. Progress in cardiovascular diseases.
Kieffer, S. K., Croci, I., Wisløff, U., & Nauman, J. (2018). Temporal Changes in a Novel Metric of Physical Activity Tracking (Personal Activity Intelligence) and Mortality: The HUNT Study, Norway. Progress in Cardiovascular Diseases.
Reitlo, L. S., Sandbakk, S. B., Viken, H., Aspvik, N. P., Ingebrigtsen, J. E., Tan, X., Wisløff, U., & Stensvold, D. (2018). Exercise patterns in older adults instructed to follow moderate-or high-intensity exercise protocol–the generation 100 study. BMC Geriatrics, 18(1), 208.
Bowen, T. S., Herz, C., Rolim, N. P., Berre, A. M. O., Halle, M., Kricke, A., Linke, A., da Silva, G. J., Wisløff, U., & Adams, V. (2018). Effects of endurance training on detrimental structural, cellular, and functional alterations in skeletal muscles of heart failure with preserved ejection fraction. Journal of cardiac failure, 24(9), 603-613.
Kieffer, S. K., Zisko, N., Coombes, J. S., Nauman, J., & Wisløff, U. (2018) Personal Activity Intelligence and Mortality in Patients with Cardiovacular Disease: The HUNT Study. Mayo Clinic Proceedings, 92(5), 1191-1201
Bozi, L. H., Takano, A. P., Campos, J. C., Rolim, N., Dourado, P. M., Voltarelli, V. A., Wisløff, U., Ferreira, J. C. B., Barreto-Chaves, M. L. M., & Brum, P. C. (2018). Endoplasmic reticulum stress impairs cardiomyocyte contractility through JNK-dependent upregulation of BNIP3. International Journal of Cardiology.
Myrstad, M., Malmo, V., Ulimoen, S. R., Tveit, A., & Loennechen, J. P. (2018). Exercise in individuals with atrial fibrillation. Clinical Research in Cardiology, 1-8.
Viken, H., Reitlo, L. S., Zisko, N., Nauman, J., Aspvik, N. P., Ingebrigtsen, J. E., Wisløff, D., & Stensvold, D. (2018). Predictors of Dropout in Exercise Trials in Older Adults. Medicine and science in sports and exercise.
Bjørnland, T., Bye, A., Ryeng, E., Wisløff, U., & Langaas, M. (2018). Powerful extreme phenotype sampling designs and score tests for genetic association studies. Statistics in medicine.
Aspvik, N. P., Viken, H., Ingebrigtsen, J. E., Zisko, N., Mehus, I., Wisløff, U., & Stensvold, D. (2018). Do weather changes influence physical activity level among older adults?–The Generation 100 study. PloS one, 13(7), e0199463.
Garnvik, L. E., Malmo, V., Janszky, I., Wisløff, U., Loennechen, J. P., & Nes, B (2018). Physical activity modifies the risk of atrial fibrillation in obese individuals: The HUNT3 study. European Journal of Preventive Cardiology. 2047487318784365
Thomsen, R. S., Nilsen, T. I., Haugeberg, G., Bye, A., Kavanaugh, A., & Hoff, M. (2019). Impact of High-Intensity Interval Training on Disease Activity and Disease in Patients With Psoriatic Arthritis: A Randomized Controlled Trial. Arthritis Care & Research, 71(4), 530-537.
Nyrnes, S. A., Garnæs, K. K., Salvesen, Ø., Timilsina, A. S., Moholdt, T., & Ingul, C. B. (2018). Cardiac function in newborns of obese women and the effect of exercise during pregnancy. A randomized controlled trial. PloS one 13(6): e0197334
Zotcheva, E., Selbæk, G., Bjertness, E., Ernstsen, L., & Strand, B. H. (2018). Leisure-time physical activity is associated with reduced risk of dementia-related mortality in adults with and without psychological distress: The Cohort of Norway. Frontiers in Aging Neuroscience, 10, 151.
Aamot, I. L., & Rognmo, Ø. (2018) Exercise therapy in intermittent claudication. E-Journal of Cardiology Practice
Carlsen, T., Salvesen, Ø., Sui, X., Lavie, C. J., Blair, S. N., Wisløff, U., & Ernstsen, L. (2018). Long-term Changes in Depressive Symptoms and Estimated Cardiorespiratory Fitness and Risk of All-Cause Mortality: The Nord-Trøndelag Health Study. Mayo Clinic Proceedings.
Tjønna, A. E., Ramos, J. S., Pressler, A., Halle, M., Jungbluth, K., Ermacora, E., Salvesen, Ø., Rodrigues, J., Bueno jr., C. R., Munk, P. S., Coombes, J., & Wisløff, U. (2018). EX-MET study: exercise in prevention on of metabolic syndrome–a randomized multicenter trial: rational and design. BMC public health, 18(1), 437.
Moholdt, T., Lavie, C. J., & Nauman, J. (2018). Sustained Physical Activity, Not Weight Loss, Associated With Improved Survival in Coronary Heart Disease. Journal of the American College of Cardiology, 71(10), 1094-1101.
Neto, M. G., Durães, A. R., Conceição, L. S. R., Saquetto, M. B., Ellingsen, Ø., & Carvalho, V. O. (2018). High intensity interval training versus moderate intensity continuous training on exercise capacity and quality of life in patients with heart failure with reduced ejection fraction: A systematic review and meta-analysis. International Journal of Cardiology.
Dias, K. A., Ingul, C. B., Tjønna, A. E., Keating, S. E., Gomersall, S. R., Follestad, T., Hosseini, M. S., Hollekim-Strand, S. M., Ro, T. B., Haram, M., & Huuse, E. M., Davies, P. S. W., Cain, P. A., Leong, G. M., & Coombes, J. S. (2017). Effect of High-Intensity Interval Training on Fitness, Fat Mass and Cardiometabolic Biomarkers in Children with Obesity: A Randomised Controlled Trial. Sports Medicine, 1-14.
Malmo, V., Kelly, A., Stolen, T., Garten, K. S., Rolim, N., Wisløff, U., Smith, G., & Loennechen, J. P. (2018). Aerobic interval training prevents age-dependent vulnerability to atrial fibrillation in rodents. Frontiers in Physiology, 9, 206.
Ingul, C. B. (2018). Low volume, high intensity: Time-efficient exercise for the treatment of hypertension. European Journal of Preventive Cardiology, 2047487318760040.
Smenes, B. T., Bækkerud, F. H., Slagsvold, K. H., Hassel, E., Wohlwend, M., Pinho, M., Høydal, M., Wisløff, U., Rognmo, Ø., & Wahba, A. (2018). Acute exercise is not cardioprotective and may induce apoptotic signalling in heart surgery: a randomized controlled trial. Interactive cardiovascular and thoracic surgery.
Ingul, C. B., Dias, K. A., Tjonna, A. E., Follestad, T., Hosseini, M. S., Timilsina, A. S., Hollekim-Strand, S. M., Ro, T. B., Davies, P. S. W., Leong, G. M., & Coombes, J. S. (2018). Effect of High Intensity Interval Training on Cardiac Function in Children with Obesity: a Randomised Controlled Trial. Progress in Cardiovascular Diseases.
Høydal, M. A., Kirkeby‐Garstad, I., Karevold, A., Wiseth, R., Haaverstad, R., Wahba, A., Stølen, T., L. Contu, R., Condorelli, G., Ellingsen, Ø., Smith, G. L., Kemi, O. J., & Wisløff, U. (2018). Human cardiomyocyte calcium handling and transverse tubules in mid‐stage of post‐myocardial‐infarction heart failure. ESC heart failure.
2017:
Williams, C. J., Williams, M. G., Eynon, N., Ashton, K. J., Little, J. P., Wisloff, U., & Coombes, J. S. (2017). Genes to predict VO 2max trainability: a systematic review. BMC genomics, 18(8), 831.
Stensvold, D., Sandbakk, S. B., Viken, H., Zisko, N., Reitlo, L. S., Nauman, J., Gaustad, S. E., Hassel, E., Moufack, M., Brønstad, E., Aspvik, N. P., Malmo, V., Steinshamn, S. L., Støylen, A., Anderssen, S. A., Helbostad, J. L., Rognmo, Ø, & Wisløff, U. (2017). Cardiorespiratory Reference Data in Older Adults: The Generation 100 Study. Medicine and science in sports and exercise, 49(11), 2206.
Bowen, T. S., Brauer, D., Rolim, N. P., Bækkerud, F. H., Kricke, A., Berre, A. M. O., Fischer, T., Linke, A., da Silva G. J., Wisløff, U., & Adams, V. (2017). Exercise Training Reveals Inflexibility of the Diaphragm in an Animal Model of Patients With Obesity‐Driven Heart Failure With a Preserved Ejection Fraction. Journal of the American Heart Association, 6(10), e006416.
Mallard, A. R., Hollekim-Strand, S. M., Coombes, J. S., & Ingul, C. B. (2017). Exercise intensity, redox homeostasis and inflammation in type 2 diabetes mellitus. Journal of science and medicine in sport, 20(10), 893-898.
Zaglia, T., Ceriotti, P., Campo, A., Borile, G., Armani, A., Carullo, P., Prando, V., Coppini, R., Vida, V., Stølen, T., Wisløff, U., Cerbai, E., Stellin, G., Faggian, G., De Stefani, D., Sandri, M., Rizzuto, R., Di Lisa, F., Pozzan, T., Catalucci, D., & Mongillo, M. (2017). Content of mitochondrial calcium uniporter (MCU) in cardiomyocytes is regulated by microRNA-1 in physiologic and pathologic hypertrophy. Proceedings of the National Academy of Sciences, 201708772.
Wisloff, U., & Lavie, C. J. (2017). Taking Physical Activity, Exercise, and Fitness to a Higher Level. Progress in cardiovascular diseases, 60(1), 1.
Wisløff, U., Lavie, C. J., & Rognmo, Ø. (2017). Letter by Wisløff et al Regarding Article,“High-Intensity Interval Training in Patients With Heart Failure With Reduced Ejection Fraction”. Circulation, 136(6), 607-608.
Leinan, I. M., Aamot, I. L., Støylen, A., Karlsen, T., & Wisløff, U. (2015). Upper arm venous compliance and fitness in stable coronary artery disease patients and healthy controls. Clinical physiology and functional imaging.
Martins C, Aschehoug I, Ludviksen M, Holst J, Finlayson G, Wisloff U, Morgan L, King N, Kulseng B. (2017). High-Intensity Interval Training, Appetite, and Reward Value of Food in the Obese. Medicine & Science in Sports & Exercise 49(9):1851-1858
D'Souza, A., Pearman, C. M., Wang, Y., Nakao, S., Logantha, S. J. R., Cox, C., Bennett, H., Zhang., Y., Johnsen, A. B., Linscheid, N., Poulsen, P. C., Elliott, J., Coulson, J., McPhee, J., Robertson, A., da Costa Martins, P. A., Kitmitto, A., Wisløff, U., Cartwright, E. J., Monfredi, O., Lundby, A., Dobrzynski, H., Ocaendy, D., Morris, G. M., & Boyett, M. R. (2017). Targeting miR-423-5p Reverses Exercise Training-Induced HCN4 Channel Remodeling and Sinus Bradycardia. Circulation research, CIRCRESAHA-117.
Dias, K. A., Masterson, C. E., Wallen, M. P., Tjonna, A. E., Hosseini, M. S., Davies, P. S., Cain, P. A., Leong, G. M., Arena, R., Ingul, C. B., & Coombes, J. S. (2017). Assessment of the 5-Minute Oxygen Uptake Efficiency Slope in Children With Obesity. Pediatric exercise science, 29(3), 350-360.
Dias, K. A., Spence, A. L., Sarma, S., Oxborough, D., Timilsina, A. S., Davies, P. S., Cain, P. A., Leong, G. M., Ingul, C. B., & Coombes, J. S. (2017). Left ventricular morphology and function in adolescents: Relations to fitness and fatness. International journal of cardiology, 240, 313-319.
Silva, G. J., Bye, A., el Azzouzi, H., & Wisløff, U. (2017). MicroRNAs as important regulators of exercise adaptation. Progress in cardiovascular diseases, 60(1), 130-151.
Sandbakk, S. B., Nauman, J., Lavie, C. J., Wisløff, U., & Stensvold, D. (2017). Combined Association of Cardiorespiratory Fitness and Body Fatness With Cardiometabolic Risk Factors in Older Norwegian Adults: The Generation 100 Study. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 1(1), 67-77.
Karlsen, T., Aamot, I. L., Haykowsky, M., & Rognmo, Ø. (2017). High Intensity Interval Training for Maximizing Health Outcomes. Progress in Cardiovascular Diseases.
Zisko, N., Skjerve, K. N., Tari, A. R., Sandbakk, S. B., Wisloff, U., Nes, B. M., & Nauman, J. (2017). Personal Activity Intelligence (PAI), Sedentary Behavior and Cardiovascular Risk Factor Clustering-The HUNT Study. Progress in Cardiovascular Diseases.
Nauman, J., Tauschek, L. C., Kaminsky, L. A., Nes, B. M., & Wisløff, U. (2017). Global fitness levels: findings from a Web-based surveillance report. Progress in Cardiovascular Diseases.
Schaardenburgh, M., Wohlwend, M., Rognmo, Ø., & Mattsson, E. J. (2017). Exercise in claudicants increase or decrease walking ability and the response relates to mitochondrial function. Journal of translational medicine, 15(1), 130.
Morland, C., Andersson, K. A., Haugen, Ø. P., Hadzic, A., Kleppa, L., Gille, A., Rinholm, J. E., Palibrk, V., Diget, E. H., Kennedy, L. H., Stølen, T., Hennestad, E., Moldestad, O., Cai, Y., Puchades, M., Offermanns, S., Vervaeke, K., Bjørås, M., Wisløff, U., Storm-Mathisen, J., & Bergersen, L. H., (2017). Exercise induces cerebral VEGF and angiogenesis via the lactate receptor HCAR1. Nature Communications, 8.
Zisko, N., Nauman, J., Sandbakk, S. B., Aspvik, N. P., Salvesen, Ø., Carlsen, T., Viken, H., Ingebrigtsen, J. E., Wisløff, U., & Stensvold, D. (2017). Absolute and relative accelerometer thresholds for determining the association between physical activity and metabolic syndrome in the older adults: The Generation-100 study. BMC geriatrics, 17(1), 109.
Karlsen, T., Nauman, J., Dalen, H., Langhammer, A., & Wisløff, U. (2017, May). The Combined Association of Skeletal Muscle Strength and Physical Activity on Mortality in Older Women: The HUNT2 Study. In Mayo Clinic Proceedings (Vol. 92, No. 5, pp. 710-718). Elsevier.
Bowen, T. S., Aakerøy, L., Eisenkolb, S., Kunth, P., Bakkerud, F., Wohlwend, M., Berre, A. M. O., Fischer, T., Wisløff, U., Schuler, G., Steinshamn, S., Adams, V, & Brønstad, E., (2017). Exercise Training Reverses Extrapulmonary Impairments in Smoke-exposed Mice. Medicine and science in sports and exercise, 49(5), 879-887.
Østhus, I. B. Ø., Lydersen, S., Dalen, H., Nauman, J., & Wisløff, U. (2017). Association of Telomere Length With Myocardial Infarction: A Prospective Cohort From the Population Based HUNT 2 Study. Progress in Cardiovascular Diseases.
Van Schaardenburgh, M., Wohlwend, M., Rognmo, Ø., & Mattsson, E. (2017). Calf raise exercise increases walking performance in patients with intermittent claudication. Journal of vascular surgery, 65(5), 1473-1482.
Hassel, E., Stensvold, D., Halvorsen, T., Wisløff, U., Langhammer, A., & Steinshamn, S. (2017). Lung function parameters improve prediction of VO2peak in an elderly population: The Generation 100 study. PloS one, 12(3), e0174058.
Ljones, K., Ness, H. O., Solvang-Garten, K., Gaustad, S. E., & Høydal, M. A. (2017). Acute exhaustive aerobic exercise training impair cardiomyocyte function and calcium handling in Sprague-Dawley rats. PloS one, 12(3), e0173449.
Nes, B. M., Gutvik, C. R., Lavie, C. J., Nauman, J., & Wisløff, U. (2017). Personalized activity intelligence (PAI) for prevention of cardiovascular disease and promotion of physical activity. The American journal of medicine, 130(3), 328-336.
Ellingsen, Ø., Halle, M., Conraads, V., Støylen, A., Dalen, H., Delagardelle, C., Larsen, A-I., Hole, T., Mezzqani, A., van Craenenbroeck E. M., Videm, V., Beckers, P. J., Christie, J. W., Winzer, E. B., Mangne, N., Woitek, F., Höllriegel, R., Pressler, A. P., Monk-Hansen, T., Snoer, M., Feiereisen, P., Valborgland, T., Kjekshus, J. K., Hambrecht, R., Gielen, S., Karlsen, T., Prescott, E. B. & Linke, A. (2017). High-Intensity Interval Training in Patients With Heart Failure With Reduced Ejection Fraction. Circulation, 135(9), 839-849.
2016:
Aspvik, N. P., Viken, H., Zisko, N., Ingebrigtsen, J. E., Wisløff, U., & Stensvold, D. (2016). Are Older Adults Physically Active Enough–A Matter of Assessment Method? The Generation 100 Study. PloS one, 11(11).
Ross, R., Blair, S. N., Arena, R., Church, T. S., Després, J. P., Franklin, B. A., Haskell, W. L., Kaminsky, L. A., Levine, B. D., Lavie, C. J., Myers, J., Niebauer, J., Sallis, R., Sawada, S. S., Sui, X., & Wisløff, U. (2016). Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation, 134(24), e653-e699.
Nauman, J., Nes, B. M., Lavie, C. J., Jackson, A. S., Sui, X., Coombes, J. S., Blair, S. N., & Wisløff, U. (2017, February). Prediction of cardiovascular mortality by estimated cardiorespiratory fitness independent of traditional risk factors: the HUNT study. In Mayo Clinic Proceedings (Vol. 92, No. 2, pp. 218-227). Elsevier.
Nes, B. M., Gutvik, C. R., Lavie, C. J., Nauman, J., & Wisløff, U. (2017). Personalized activity intelligence (PAI) for prevention of cardiovascular disease and promotion of physical activity. The American journal of medicine, 130(3), 328-336.
Egerton, T., Helbostad, J. L., Stensvold, D., & Chastin, S. F. (2016). Fatigue alters the pattern of physical activity behavior in older adults: observational analysis of data from the Generation 100 Study. Journal of aging and physical activity, 24(4), 633-64
van Schaardenburgh, M., Wohlwend, M., Rognmo, Ø., & Mattsson, E. J. (2016). Mitochondrial respiration after one session of calf raise exercise in patients with peripheral vascular disease and healthy older adults. PLoS One, 11(10).
Sandbakk, S. B., Nauman, J., Zisko, N., Sandbakk, Ø., Aspvik, N. P., Stensvold, D., & Wisløff, U. (2016, November). Sedentary time, cardiorespiratory fitness, and cardiovascular risk factor clustering in older adults--the Generation 100 study. In Mayo Clinic Proceedings (Vol. 91, No. 11, pp. 1525-1534). Elsevier.
Seiler, M., Bowen, T. S., Rolim, N., Dieterlen, M. T., Werner, S., Hoshi, T., Fischer, T., Mangner, N., Linke, A., Schuler, G., Halle, M., Wisløff, U., & Adams, V. (2016). Skeletal muscle alterations are exacerbated in heart failure with reduced compared with preserved ejection fraction: mediated by circulating cytokines?. Circulation: Heart Failure, 9(9), e003027
Skaug, E. A., Nes, B., Aspenes, S. T., & Ellingsen, Ø. (2016). Non-smoking tobacco affects endothelial function in healthy men in one of the largest health studies ever performed; The Nord-Trøndelag Health Study in Norway; HUNT3. PloS one, 11(8).
Martins, C., Kazakova, I., Ludviksen, M., Mehus, I., Wisloff, U., Kulseng, B., Morgan, L., & King, N. (2016). High-intensity interval training and isocaloric moderate-intensity continuous training result in similar improvements in body composition and fitness in obese individuals. International journal of sport nutrition and exercise metabolism, 26(3), 197-204.
Bozi, L. H., Jannig, P. R., Rolim, N., Voltarelli, V. A., Dourado, P. M., Wisløff, U., & Brum, P. C. (2016). Aerobic exercise training rescues cardiac protein quality control and blunts endoplasmic reticulum stress in heart failure rats. Journal of cellular and molecular medicine, 20(11), 2208-2212.
Malmo, V., Langhammer, A., Bønaa, K. H., Loennechen, J. P., & Ellekjaer, H. (2016). Validation of self-reported and hospital-diagnosed atrial fibrillation: the HUNT study. Clinical epidemiology, 8, 185.
Wallen, M. P., Gomersall, S. R., Keating, S. E., Wisløff, U., & Coombes, J. S. (2016). Accuracy of heart rate watches: implications for weight management. PloS one, 11(5)
Høydal, M. A., Stølen, T. O., Kettlewell, S., Maier, L. S., Brown, J. H., Sowa, T., Catalucci, D., Condorelli, G., Kemi, O. J., Smith, G. L., & Wisløff, U. (2016). Exercise training reverses myocardial dysfunction induced by CaMKIIδC overexpression by restoring Ca2+ homeostasis. Journal of Applied Physiology, 121(1), 212-220.
Revdal, A., Hollekim-Strand, S. M., & Ingul, C. B. (2016). Can time efficient exercise improve cardiometabolic risk factors in type 2 diabetes? A pilot study. Journal of sports science & medicine, 15(2), 308.
Bye, A., Røsjø, H., Nauman, J., Silva, G. J., Follestad, T., Omland, T., & Wisløff, U. (2016). Circulating microRNAs predict future fatal myocardial infarction in healthy individuals–The HUNT study. Journal of molecular and cellular cardiology, 97, 162-168.
Chapman, R. F., Karlsen, T., Ge, R. L., Stray-Gundersen, J., & Levine, B. D. (2016). Living altitude influences endurance exercise performance change over time at altitude. Journal of Applied Physiology, 120(10), 1151-1158.
Lauglo, R., Vik, T., Lamvik, T., Stensvold, D., Finbråten, A. K., & Moholdt, T. (2016). High-intensity interval training to improve fitness in children with cerebral palsy. BMJ open sport & exercise medicine, 2(1), e000111.
Dias, K. A., Coombes, J. S., Green, D. J., Gomersall, S. R., Keating, S. E., Tjonna, A. E., Hollekim-Strand, S. M., Hosseini, M. S., Ro, T. B., Haram, M., Huuse, E. M., Davies, P. S. W., Cain, P. A., Leong, G. M., & Ingul, C. B. (2016). Effects of exercise intensity and nutrition advice on myocardial function in obese children and adolescents: a multicentre randomised controlled trial study protocol. BMJ open, 6(4), e010929
Halle, M., Adams, V., Edelmann, F., Pieske, B., & Wisløff, U. (2016). Benefit of exercise in atrial fibrillation: diastolic function matters!. Journal of the American College of Cardiology, 67(10), 1257-1258.
Hollekim-Strand, S. M., Høydahl, S. F., Follestad, T., Dalen, H., Bjørgaas, M. R., Wisløff, U., & Ingul, C. B. (2016). Exercise training normalizes timing of left ventricular untwist rate, but not peak untwist rate, in individuals with type 2 diabetes and diastolic dysfunction: a pilot study. Journal of the American Society of Echocardiography, 29(5), 421-430.
Loe, H., Nes, B. M., & Wisløff, U. (2016). Predicting VO2peak from submaximal-and peak exercise models: the HUNT 3 fitness study, Norway. PloS one, 11(1).
Malmo, V., Nes, B. M., Amundsen, B. H., Tjonna, A. E., Stoylen, A., Rossvoll, O., Wisløff, U. & Loennechen, J. P. (2016). Aerobic interval training reduces the burden of atrial fibrillation in the short term: a randomized trial. Circulation, 133(5), 466-473.
2015:
Hassel, E., Stensvold, D., Halvorsen, T., Wisløff, U., Langhammer, A., & Steinshamn, S. (2015). Association between pulmonary function and peak oxygen uptake in elderly: the Generation 100 study. Respiratory research, 16(1), 1-8.
Leinan, I. M., Aamot, I. L., Støylen, A., Karlsen, T., & Wisløff, U. (2017). Upper arm venous compliance and fitness in stable coronary artery disease patients and healthy controls. Clinical physiology and functional imaging, 37(5), 498-506.
Wisløff, U., Coombes, J. S., & Rognmo, Ø. (2015). CrossTalk proposal: high intensity interval training does have a role in risk reduction or treatment of disease. The Journal of physiology, 593(24), 5215.
- Wisløff, U., Coombes, J. S., & Rognmo, Ø. (2015). Rebuttal from Ulrik Wisløff, Jeff Coombes and Øivind Rognmo. The Journal of physiology, 593(24), 5223.
Nauman, J., Stensvold, D., Coombes, J. S., & Wisløff, U. (2016). Cardiorespiratory Fitness, Sedentary Time, and Cardiovascular Risk Factor Clustering. Medicine and science in sports and exercise, 48(4), 625-632.
Viken, H., Aspvik, N. P., Ingebrigtsen, J. E., Zisko, N., Wisløff, U., & Stensvold, D. (2016). Correlates of objectively measured physical activity among Norwegian older adults: the generation 100 study. Journal of aging and physical activity, 24(3), 369-375.
Baekkerud, F. H., Solberg, F., Leinan, I. M., Wisløff, U., Karlsen, T., & Rognmo, Ø. (2016). Comparison of three popular exercise modalities on V˙ O2max in overweight and obese. Medicine & Science in Sports & Exercise, 48(3), 491-498.
Adams, V., Alves, M., Fischer, T., Rolim, N., Werner, S., Schütt, N., Bowen, T. S., Linke, A., Schuler, G. & Wisloff, U. (2015). High-intensity interval training attenuates endothelial dysfunction in a Dahl salt-sensitive rat model of heart failure with preserved ejection fraction. Journal of Applied Physiology, 119(6), 745-752.
Bakker, E., Engan, H., Patrician, A., Schagatay, E., Karlsen, T., Wisløff, U., & Gaustad, S. E. (2015). Acute dietary nitrate supplementation improves arterial endothelial function at high altitude: a double-blinded randomized controlled cross over study. Nitric Oxide, 50, 58-64.
Ernstsen, L., Rangul, V., Nauman, J., Nes, B. M., Dalen, H., Krokstad, S., Lavie, C. J., Blair, S. N., & Wisløff, U. (2016). Protective effect of regular physical activity on depression after myocardial infarction: the HUNT study. The American journal of medicine, 129(1), 82-88.
Hollekim-Strand, S. M., Malmo, V., Follestad, T., Wisløff, U., & Ingul, C. B. (2015). Fast food increases postprandial cardiac workload in type 2 diabetes independent of pre-exercise: A pilot study. Nutrition journal, 14(1), 1-11.
Zisko, N., Carlsen, T., Salvesen, Ø., Aspvik, N. P., Ingebrigtsen, J. E., Wisløff, U., & Stensvold, D. (2015). New relative intensity ambulatory accelerometer thresholds for elderly men and women: the Generation 100 study. BMC geriatrics, 15(1), 1-10.
Hagen, K., Wisløff, U., Ellingsen, Ø., Stovner, L. J., & Linde, M. (2016). Headache and peak oxygen uptake: The HUNT3 study. Cephalalgia, 36(5), 437-444.
Karlsen, T., Leinan, I. M., Aamot, I. L., Dalen, H., & Støylen, A. (2016). Safety of the CO-rebreathing method in patients with coronary artery disease. Medicine and science in sports and exercise, 48(1), 33-38.
Rolim, N., Skårdal, K., Høydal, M., Sousa, M. M., Malmo, V., Kaurstad, G., Ingul, C. B., Hansen, H. E. M., Alves, M. N., Thuen, M., Haraldseth, O., Brum, P. C., Slupphaug, G., Loennechen, J. P., Stølen, T., & Wisløff, U. (2015). Aerobic interval training reduces inducible ventricular arrhythmias in diabetic mice after myocardial infarction. Basic research in cardiology, 110(4), 1-10.
Kraljevic, J., Høydal, M. A., Ljubkovic, M., Moreira, J. B., Jørgensen, K., Ness, H. O., Bækkerud, F. H., Zeljko, D., Wisløff, U., & Marinovic, J. (2015). Role of KATP Channels in Beneficial Effects of Exercise in Ischemic Heart Failure. Medicine and science in sports and exercise, 47(12), 2504-2512.
Dalen, T., Ingebrigtsen, J., Ettema, G., Hjelde, G. H., & Wisløff, U. (2016). Player load, acceleration, and deceleration during forty-five competitive matches of elite soccer. The Journal of Strength & Conditioning Research, 30(2), 351-359.
Sandstad, J., Stensvold, D., Hoff, M., Nes, B. M., Arbo, I., & Bye, A. (2015). The effects of high intensity interval training in women with rheumatic disease: a pilot study. European journal of applied physiology, 115(10), 2081-2089.
Madssen, E., Videm, V., Moholdt, T., Wisløff, U., Hegbom, K., & Wiseth, R. (2015). Predictors of beneficial coronary plaque changes after aerobic exercise. Medicine and science in sports and exercise, 47(11), 2251-2256.
Zisko, N., Stensvold, D., Hordnes-Slagsvold, K., Rognmo, Ø., Nauman, J., Wisløff, U., & Karlsen, T. (2015). Effect of change in VO2max on daily total energy expenditure in a cohort of Norwegian men: a randomized pilot study. The open cardiovascular medicine journal, 9, 50.
Lund, J., Hafstad, A. D., Boardman, N. T., Rossvoll, L., Rolim, N. P., Ahmed, M. S., ... & Aasum, E. (2015). Exercise training promotes cardioprotection through oxygen-sparing action in high fat-fed mice. American Journal of Physiology-Heart and Circulatory Physiology, 308(8), H823-H829.
Leinan, I. M., Grønnevik, Ø., Støylen, A., Wisløff, U., & Karlsen, T. (2015). A cross sectional study of arm venous compliance in fit healthy subjects. Journal of Cardiovascular Research, 1(2).
Wisløff, U., Bye, A., Stølen, T., Kemi, O. J., Pollott, G. E., Pande, M., McEachin, R. C., Britton, S. L., & Koch, L. G. (2015). Blunted cardiomyocyte remodeling response in exercise-resistant rats. Journal of the American College of Cardiology, 65(13), 1378-1380.
Moreira, J. B., Wohlwend, M., Alves, M. N., Wisløff, U., & Bye, A. (2015). A small molecule activator of AKT does not reduce ischemic injury of the rat heart. Journal of translational medicine, 13(1), 1-10.
Karlsen, T., Leinan, I. M., Bækkerud, F. H., Lundgren, K. M., Tari, A., Steinshamn, S. L., Støylen, A., & Rognmo, Ø. (2015). How to be 80 year old and have a VO2max of a 35 year old. Case reports in medicine, 2015.
Aamot, I. L., Karlsen, T., Dalen, H., & Støylen, A. (2016). Long‐term exercise adherence after high‐intensity interval training in cardiac rehabilitation: a randomized study. Physiotherapy Research International, 21(1), 54-64.
Stensvold, D., Viken, H., Rognmo, Ø., Skogvoll, E., Steinshamn, S., Vatten, L. J., Coombes, J. S., Anderssen, S. A., Magnussen, J., Ingebrigtsen, J. E., Singh, M. A. F., Langhammer, A., Støylen, A., Helbostad, J. L., & Wisløff, U. (2015). A randomised controlled study of the long-term effects of exercise training on mortality in elderly people: study protocol for the Generation 100 study. BMJ open, 5(2), e007519.
Lundgren, K. M., Karlsen, T., Sandbakk, Ø., James, P. E., & Tjønna, A. E. (2015). Sport-specific physiological adaptations in highly trained endurance athletes. Medicine and science in sports and exercise, 47(10), 2150-2157.
Bowen, T. S., Rolim, N. P., Fischer, T., Bækkerud, F. H., Medeiros, A., Werner, S., Brønstd, E., Rognmo, Ø., Mangner, N., Linke, A., Schuler, G., Silva, G. J. J., Wisløff, U., Adams, V., & Optimex Study Group. (2015). Heart failure with preserved ejection fraction induces molecular, mitochondrial, histological, and functional alterations in rat respiratory and limb skeletal muscle. European journal of heart failure, 17(3), 263-272.
Berendoncks, A. M. V., Stensvold, D., Garnier, A., Fortin, D., Sente, T., Vrints, C. J., Slørdahl, S. A., Ventura-Clapier, R., Wisløff, U., & Conraads, V. M. (2015). Disturbed adiponectin–AMPK system in skeletal muscle of patients with metabolic syndrome. European journal of preventive cardiology, 22(2), 203-205.
Martins, C., Stensvold, D., Finlayson, G., Holst, J., Wisloff, U., Kulseng, B., Morgan, L. & King, N. (2015). Effect of moderate-and high-intensity acute exercise on appetite in obese individuals. Medicine and Science in Sports and Exercise, 47(1), 40-48.
2014:
Loe, H., Steinshamn, S., & Wisløff, U. (2014). Cardio-respiratory reference data in 4631 healthy men and women 20-90 years: the HUNT 3 fitness study. PloS one, 9(11), e113884.
Suchy, C., Massen, L., Rognmo, Ø., Van Craenenbroeck, E. M., Beckers, P., Kraigher-Krainer, E., Linke, A., Adams, V., Wisløff, U., Pieske, B., & Halle, M. (2014). Optimising exercise training in prevention and treatment of diastolic heart failure (OptimEx-CLIN): rationale and design of a prospective, randomised, controlled trial. European journal of preventive cardiology, 21(2_suppl), 18-25.
Slagsvold, K. H., Moreira, J. B., Rognmo, Ø., Høydal, M., Bye, A., Wisløff, U., & Wahba, A. (2014). Remote ischemic preconditioning preserves mitochondrial function and activates pro-survival protein kinase Akt in the left ventricle during cardiac surgery: a randomized trial. International journal of cardiology, 177(2), 409-417.
Hollekim-Strand, S. M., Bjørgaas, M. R., Albrektsen, G., Tjønna, A. E., Wisløff, U., & Ingul, C. B. (2014). High-intensity interval exercise effectively improves cardiac function in patients with type 2 diabetes mellitus and diastolic dysfunction: a randomized controlled trial. Journal of the American College of Cardiology, 64(16), 1758-1760.
Hassel, E., Berre, A. M., Skjulsvik, A. J., & Steinshamn, S. (2014). Effects of exercise training on pulmonary vessel muscularization and right ventricular function in an animal model of COPD. Respiratory research, 15(1), 1-8.
Madssen, E., Arbo, I., Granøien, I., Walderhaug, L., & Moholdt, T. (2014). Peak oxygen uptake after cardiac rehabilitation: a randomized controlled trial of a 12-month maintenance program versus usual care. PLoS One, 9(9), e107924.
Monfredi, O., Lyashkov, A. E., Johnsen, A. B., Inada, S., Schneider, H., Wang, R., Nirmalan, M., Wisløff, U., Maltsel, V. A., Lakatta, E. G., Zhang, H., & Boyett, M. R. (2014). Biophysical characterization of the underappreciated and important relationship between heart rate variability and heart rate. Hypertension, 64(6), 1334-1343.
Slagsvold, K. H., Johnsen, A. B., Rognmo, Ø., Høydal, M., Wisløff, U., & Wahba, A. (2014). Comparison of left versus right atrial myocardium in patients with sinus rhythm or atrial fibrillation–an assessment of mitochondrial function and microRNA expression. Physiological reports, 2(8), e12124.
Madssen, E., Moholdt, T., Videm, V., Wisløff, U., Hegbom, K., & Wiseth, R. (2014). Coronary atheroma regression and plaque characteristics assessed by grayscale and radiofrequency intravascular ultrasound after aerobic exercise. The American journal of cardiology, 114(10), 1504-1511.
Pedersen, L. R., Olsen, R. H., Jürs, A., Astrup, A., Chabanova, E., Simonsen, L., Wisløff, U., Haugaard, S. B., & Prescott, E. (2015). A randomised trial comparing weight loss with aerobic exercise in overweight individuals with coronary artery disease: The CUT-IT trial. European journal of preventive cardiology, 22(8), 1009-1017.
Ingebrigtsen, J., Dalen, T., Hjelde, G. H., Drust, B., & Wisløff, U. (2015). Acceleration and sprint profiles of a professional elite football team in match play. European journal of sport science, 15(2), 101-110.
Skaug, E. A., Madssen, E., Aspenes, S. T., Wisløff, U., & Ellingsen, Ø. (2014). Cardiovascular risk factors have larger impact on endothelial function in self-reported healthy women than men in the HUNT3 Fitness study. PLoS One, 9(7), e101371.
Nes, B. M., Karlsen, T., Rognmo, Ø., & Wisløff, U. (2014). Comparing Cardiorespiratory Fitness Across Populations. Chest, 146(1), e30.
Nes, B. M., Vatten, L. J., Nauman, J., Janszky, I., & Wisløff, U. (2014). A simple nonexercise model of cardiorespiratory fitness predicts long-term mortality. Medicine and science in sports and exercise, 46(6), 1159-1165.
Martins, C., Stensvold, D., Finlayson, G., Holst, J., Wisloff, U., Kulseng, B., Morgan, L. & King, N. (2015). Effect of moderate-and high-intensity acute exercise on appetite in obese individuals. Medicine and Science in Sports and Exercise, 47(1), 40-48.
Slagsvold, K. H., Johnsen, A. B., Rognmo, Ø., Høydal, M. A., Wisløff, U., & Wahba, A. (2014). Mitochondrial respiration and microRNA expression in right and left atrium of patients with atrial fibrillation. Physiological genomics, 46(14), 505-511.
D’Souza, A., Bucchi, A., Johnsen, A. B., Logantha, S. J. R., Monfredi, O., Yanni, J., Prehar, S., Hart, G., Cartwright, E., Wisløff, U., Dobryznski, H., DiFrancesco, D., Morris, G. M., & Boyett, M. R. (2014). Exercise training reduces resting heart rate via downregulation of the funny channel HCN4. Nature communications, 5(1), 1-12.
Moholdt, T., Wisløff, U., Lydersen, S., & Nauman, J. (2014). Current physical activity guidelines for health are insufficient to mitigate long-term weight gain: more data in the fitness versus fatness debate (The HUNT study, Norway). British Journal of Sports Medicine, 48(20), 1489-1496.
Chapman, R. F., Karlsen, T., Resaland, G. K., Ge, R. L., Harber, M. P., Witkowski, S., Stray-Gundersen, J., & Levine, B. D. (2014). Defining the “dose” of altitude training: how high to live for optimal sea level performance enhancement. Journal of applied physiology, 116(6), 595-603.
Røsjø, H., Dahl, M. B., Bye, A., Andreassen, J., Jørgensen, M., Wisløff, U., Christensen, G., Edvardsen, T., & Omland, T. (2014). Prognostic value of circulating microRNA-210 levels in patients with moderate to severe aortic stenosis. PLoS One, 9(3), e91812.
Hatle, H., Støbakk, P. K., Mølmen, H. E., Brønstad, E., Tjønna, A. E., Steinshamn, S., Skogvoll, E., Wisløff, U., Ingul, C. B., & Rognmo, Ø. (2014). Effect of 24 sessions of high-intensity aerobic interval training carried out at either high or moderate frequency, a randomized trial. PloS one, 9(2), e88375.
Jannig, P. R., Moreira, J. B., Bechara, L. R., Bozi, L. H., Bacurau, A. V., Monteiro, A. W., Dourado, P. M., Wisløff, U., & Brum, P. C. (2014). Autophagy signaling in skeletal muscle of infarcted rats. PLoS One, 9(1), e85820.
2013:
Slagsvold, K. H., Rognmo, Ø., Høydal, M., Wisløff, U., & Wahba, A. (2014). Remote ischemic preconditioning preserves mitochondrial function and influences myocardial microRNA expression in atrial myocardium during coronary bypass surgery. Circulation research, 114(5), 851-859.
Askim, T., Dahl, A. E., Aamot, I. L., Hokstad, A., Helbostad, J., & Indredavik, B. (2014). High‐intensity aerobic interval training for patients 3–9 months after stroke. A feasibility study. Physiotherapy research international, 19(3), 129-139.
Pedersen, L. R., Olsen, R. H., Frederiksen, M., Astrup, A., Chabanova, E., Hasbak, P., Holst, J. J., Kjær, A., Newman, J. W., Walzem, R., Wisløff, U., Sajadieh, A., Haugaard, S. B., & Prescott, E. (2013). Copenhagen study of overweight patients with coronary artery disease undergoing low energy diet or interval training: the randomized CUT-IT trial protocol. BMC cardiovascular disorders, 13(1), 1-8.
Weston, K. S., Wisløff, U., & Coombes, J. S. (2014). High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. British journal of sports medicine, 48(16), 1227-1234.
Johnsen, A. B., Rolim, N. P., Stølen, T., Alves, M., Sousa, M. M., Slupphaug, G., Britton, S. L., Koch, L. G., Smith, G. L., Wisløff, U., & Høydal, M. A. (2013). Atrial myocyte function and Ca2+ handling is associated with inborn aerobic capacity. PLoS One, 8(10), e76568.
Berendoncks, A. M. V., Stensvold, D., Garnier, A., Fortin, D., Sente, T., Vrints, C. J., Slørdahl, S. A., Ventura-Clapier, R., & Conraads, V. M. (2015). Disturbed adiponectin–AMPK system in skeletal muscle of patients with metabolic syndrome. European journal of preventive cardiology, 22(2), 203-205.
Raschke, S., Elsen, M., Gassenhuber, H., Sommerfeld, M., Schwahn, U., Brockmann, B., Jung, R., Wisløff, U., Tjønna, A. E., Raastad, T., Hallén, J., Norheim, F., Drevon, C. A., Romacho, T., Eckardt, K., & Eckel, J. (2013). Evidence against a beneficial effect of irisin in humans. PloS one, 8(9), e73680.
Moholdt, T., Madssen, E., Rognmo, Ø., & Aamot, I. L. (2014). The higher the better? Interval training intensity in coronary heart disease. Journal of science and medicine in sport, 17(5), 506-510.
Aamot, I. L., Forbord, S. H., Karlsen, T., & Støylen, A. (2014). Does rating of perceived exertion result in target exercise intensity during interval training in cardiac rehabilitation? A study of the Borg scale versus a heart rate monitor. Journal of science and medicine in sport, 17(5), 541-545.
Aamot, I. L., Forbord, S. H., Gustad, K., Løckra, V., Stensen, A., Berg, A. T., Dalen, H., Karlsen, T., & Støylen, A. (2014). Home-based versus hospital-based high-intensity interval training in cardiac rehabilitation: a randomized study. European journal of preventive cardiology, 21(9), 1070-1078.
Johnsen, A. B., Høydal, M., Røsbjørgen, R., Stølen, T., & Wisløff, U. (2013). Aerobic interval training partly reverse contractile dysfunction and impaired Ca2+ handling in atrial myocytes from rats with post infarction heart failure. PLoS One, 8(6), e66288.
Tjønna, A. E., Leinan, I. M., Bartnes, A. T., Jenssen, B. M., Gibala, M. J., Winett, R. A., & Wisløff, U. (2013). Low-and high-volume of intensive endurance training significantly improves maximal oxygen uptake after 10-weeks of training in healthy men. PloS one, 8(5), e65382.
Rognmo, Ø., Moholdt, T., Bakken, H., Hole, T., Mølstad, P., Myhr, N. E., Grimsmo, J., & Wisløff, U. (2013). Response to letter regarding article,“Cardiovascular risk of high-versus moderate-intensity aerobic exercise in coronary heart disease patients”. Circulation, 127(21), e638-e638.
Loe, H., Rognmo, Ø., Saltin, B., & Wisløff, U. (2013). Aerobic capacity reference data in 3816 healthy men and women 20–90 years. PloS one, 8(5), e64319.
Moreira, J. B., Bechara, L. R., Bozi, L. H., Jannig, P. R., Monteiro, A. W., Dourado, P. M., Wisløff, U., & Brum, P. C. (2013). High-versus moderate-intensity aerobic exercise training effects on skeletal muscle of infarcted rats. Journal of Applied Physiology, 114(8), 1029-1041.
Solberg, A., Robertson, A. B., Aronsen, J. M., Rognmo, Ø., Sjaastad, I., Wisløff, U., & Klungland, A. (2013). Deletion of mouse Alkbh7 leads to obesity. Journal of molecular cell biology, 5(3), 194-203.
Kraljevic, J., Marinovic, J., Pravdic, D., Zubin, P., Dujic, Z., Wisloff, U., & Ljubkovic, M. (2013). Aerobic interval training attenuates remodelling and mitochondrial dysfunction in the post-infarction failing rat heart. Cardiovascular research, 99(1), 55-64.
Bye, A., Røsjø, H., Aspenes, S. T., Condorelli, G., Omland, T., & Wisløff, U. (2013). Circulating microRNAs and aerobic fitness–the HUNT-Study. PloS one, 8(2), e57496.
Rehn, T. A., Winett, R. A., Wisløff, U., & Rognmo, Ø. (2013). Increasing physical activity of high intensity to reduce the prevalence of chronic diseases and improve public health. The open cardiovascular medicine journal, 7, 1.
Kemi, O. J., Haram, P. M., Høydal, M. A., Wisløff, U., & Ellingsen, Ø. (2013). Exercise training and losartan improve endothelial function in heart failure rats by different mechanisms. Scandinavian Cardiovascular Journal, 47(3), 160-167.
Strand, L. B., Laugsand, L. E., Wisløff, U., Nes, B. M., Vatten, L., & Janszky, I. (2013). Insomnia symptoms and cardiorespiratory fitness in healthy individuals: The Nord-Trøndelag Health Study (HUNT). Sleep, 36(1), 99-108.
Send us an e-mail:
cerg-post@mh.ntnu.no
Send us regular mail:
NTNU, Fakultet for medisin og helsevitenskap
Institutt for sirkulasjon og bildediagnostikk
Postboks 8905
7491 Trondheim
Visit us:
St. Olavs Hospital
Prinsesse Kristinas gt. 3
Akutten og Hjerte-lunge-senteret, 3. etg.
7006 Trondheim